|
Fortunately, lesions of the lumbar and sacral plexuses
(heretofore collectively referred to as the lumbosacral plexus)
and the proximal sciatic nerve are infrequent. Unfortunately, an
inappropriately conservative approach is often undertaken in
patients harboring these lesions because of the suspected degree
of difficulty of the surgical approach. The bony and soft-tissue
confines of the peritoneal cavity, retroperitoneum, pelvis, and
gluteal region result in the application of the term
"no-man's-land" to the region of the lumbosacral plexus and the
proximal sciatic nerve.
Indications
for surgery of nerves in this no-man's-land include tumors
(usually nerve sheath tumors), traumatic injuries (including
penetrating, stretch, and injection injuries), and, rarely,
surgery for neural ablation. Seven fundamental surgical
approaches to the lumbosacral plexus and the proximal sciatic
nerve exist. Anyone or combination of these approaches may be
used to expose a specific portion of this region. A combination
of approaches (discussion follows sections on each of the seven
approaches listed below) may be used when a long longitudinal
exposure is indicated or when a lesion exists in a transition
zone from one surgical approach to another. The seven surgical
approaches are as follows:
1. A wide
foraminotomy approach to the proximal nerve roots (to gain
access to the proximal nerve roots as they exit the dural sac
and the spinal canal)
2.
The lateral extracavitary approach to the spine (to expose the
nerve roots within the spinal canal, as well as approximately
4-6 cm lateral to the neuroforamina)
3. The
anterolateral extraperitoneal approach to the spine (to expose
the proximal mid- to lower-retroperitoneal lumbar region)
4. The
pelvic brim extraperitoneal approach (to expose retroperitoneal
lesions located in the low lumbar region)
5. The
Pfannenstiel infraperitoneal approach (to expose caudal
infraperitoneal lesions within the pelvis)
6. The
transperitoneal approach (to expose, for the most part, the
regions approached via approaches 3-5)
7. The
extrapelvic infragluteal approach (to expose the proximal
sciatic nerve as it exits from the pelvis through the sciatic
notch into the infragluteal space)
With
an aggressive surgical approach, there is no absolute
no-man's-land in the entire region of the lumbar and sacral
plexuses and the proximal sciatic nerve, although regions that
could be considered "relative no-man's-lands" do exist (i.e. the
region of the sciatic nerve that is located within 2-3 cm of the
sciatic notch). An understanding of the regional anatomy
enhances one's ability to expose this region of the nervous
system (several nicely done radiographic studies have enhanced
the awareness of clinicians with
regard to the understanding of the anatomy), In order to further
enhance this understanding, the surgical approach to each of
these seven regions will be discussed. A discussion of
appropriate combined approaches and the indications for these
surgical approaches will also be presented.
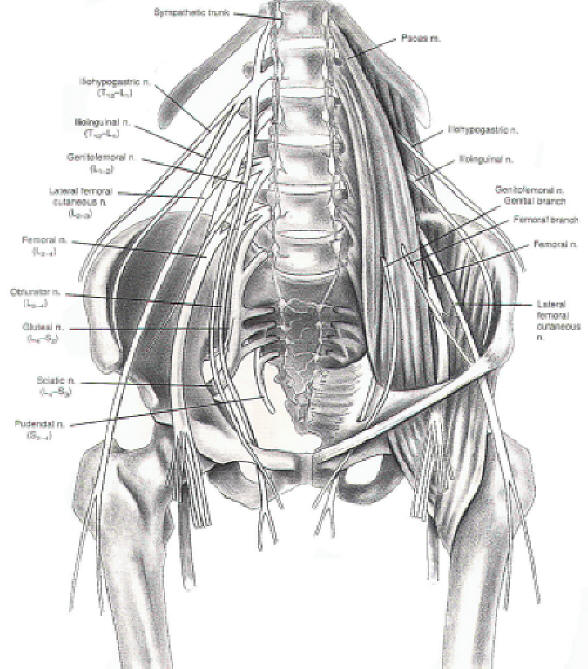
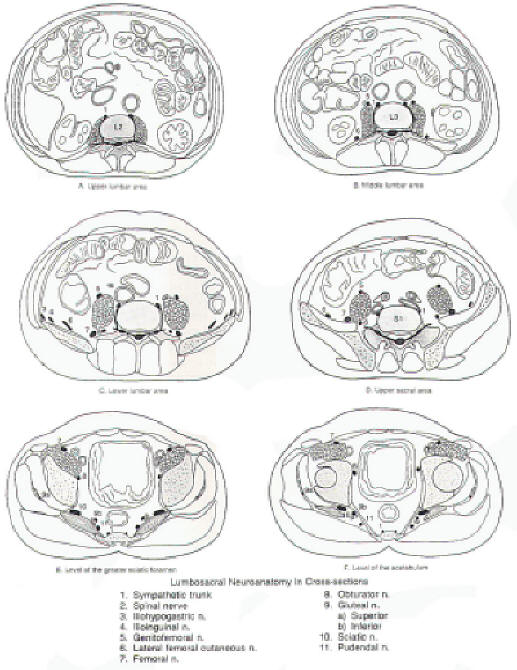
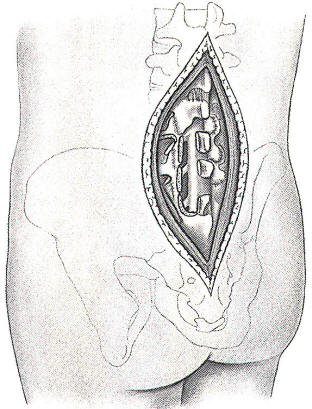
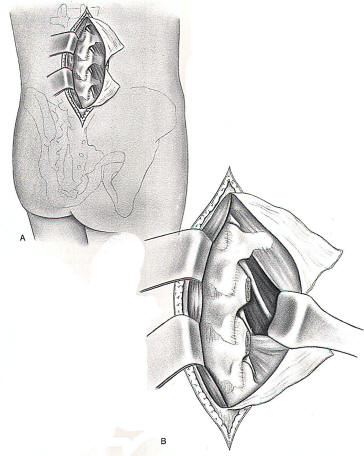
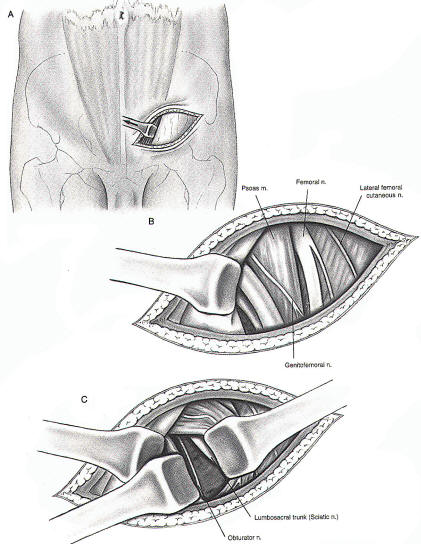
Figure 1
illustrates the lumbosacral plexus and its relationship to
surrounding tissues. Figure 2 illustrates the axial anatomy of
the lumbosacral plexus at a variety of levels. A correlation of
Figures 1 and 2 should allow for an understanding of the
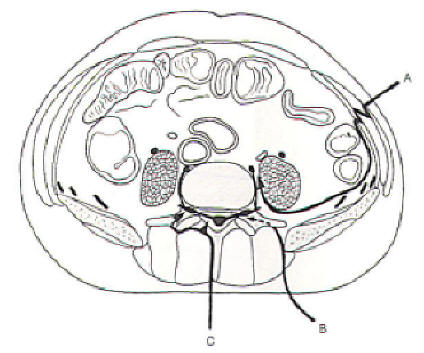
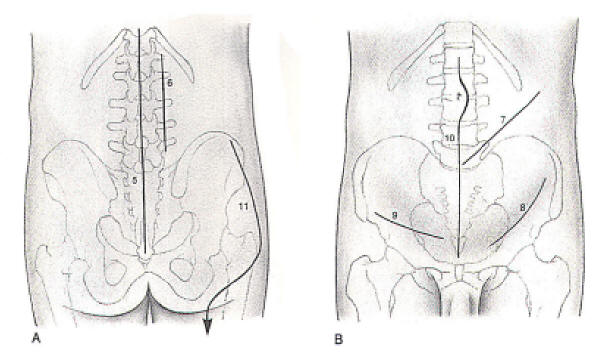
three-dimensional anatomy of the lumbosacral plexus. The planes
of dissection of several of the approaches for lumbosacral
plexus exposure presented herein are illustrated in Figure 3.
whereas Figure 4 illustrates the incisions used for the surgical
exposures. A clear understanding of these planes is absolutely
necessary before a surgical undertaking of anyone of these
approaches is entertained.
 |
 |
| Fig-1 |
Fig-2 |
 |
 |
| Fig-3 |
Fig-4 |
|
 Wide
Foraminotomy Approach to the Proximal Nerve Roots
Wide
Foraminotomy Approach to the Proximal Nerve Roots
The midline
exposure of the lumbar and upper sacral spine allows access to
roughly the proximal 1-2 cm of the nerve roots as they exit the
spinal canal, as well as the segment of the nerve root within
the canal (Figure 5), One may approach this region with a
lateral subperiosteal dissection, followed by a laminectomy or
hemilaminectomy using standard spinal surgical techniques. The
nerve root is then visualized within the spinal canal. Following
further bone removal, the neuroforamina may be unroofed and the
nerve root followed distally for approximately 1-2 cm. A more
lateral approach with extensive lateral paraspinous muscle
retraction or splitting with soft-tissue dissection can be
performed without the removal of the facet joint. This gains
access to the more distal aspect of the nerve root approachable
from this operation. The preservation of the integrity of the
facet joint should be accomplished when possible. Subsequent
degenerative changes, instability, and pain may be related to
excessive bone removal in this region. If the facet joint is
disrupted, the performance of a spinal fusion (either interbody
or lateral) is a consideration. The advantages of the wide
foraminotomy approach to the posterior spine include the
familiarity of the region to spine surgeons and the relatively
uncomplicated nature of the surgical exposure. The disadvantages
of this approach include its limited exposure. Only the very
proximal portion of the nerve root is accessible by this
approach.
|
 |
| Fig-5 |
|
 Lateral
Extracavitary Approach to the Proximal Lumbosacral Plexus
Lateral
Extracavitary Approach to the Proximal Lumbosacral Plexus
The lateral
extracavitary approach to the spine can be used to gain access
to the first 6 cm of the extradural lumbar nerve roots (Figure
6). All regions of the thoracic and lumbar spine can be
approached with this operation, although surgical exposure of
the lower lumbar region via the lateral extracavitary approach
requires significant dorsal ilium resection. The three-quarter
prone position is preferred by this author because it
facilitates visualization of the surgical field by the surgeon.
It simultaneously minimizes blood loss (due to lessened
abdominal compression).
The spine
is approached through either a midline-oriented hockey-stick
flap incision or through a paramedian longitudinal incision. A
paramedian longitudinal incision is perhaps most appropriate for
nerve exploration. Midline spinal exposure is not required for
this operation; therefore, the creation of a cutaneous flap,
with all its attendant risks, is not warranted. The
thoracodorsal fascia is incised following its exposure. The
erector spinae muscle is reflected medially following separation
from the quadratus lumborum muscle. A well-defined plane exists
between these two muscles (the middle layer of the thoracolumbar
fascia). This plane is followed medially, allowing exposure of
the transverse processes. Subperiosteal dissection along the
underside of the transverse process allows one to follow the
under surface of the transverse process, along the pedicle and
the vertebral body, without fear of injury to the nerve roots as
they exit the spinal canal. Following this exposure, the nerve
roots can be isolated as they exit from the neuroforamina into
the psoas muscle. This exposure is difficult due to the
requisite muscle splitting. The nerves do not course between
tissue planes in this region, thus necessitating the
aforementioned muscle splitting. Further retraction laterally
will allow access to the first 6 cm of the nerve after its exit
from the spinal canal.
The
advantages of this approach include the lack of intrapelvic
dissection required and the ability to extend the dissection
farther laterally than allowed with a wide foraminotomy
approach. The disadvantages include the difficulties of
dissecting across tissue planes and the resultant soft-tissue
trauma incurred.
|
 |
| Fig-6 |
|
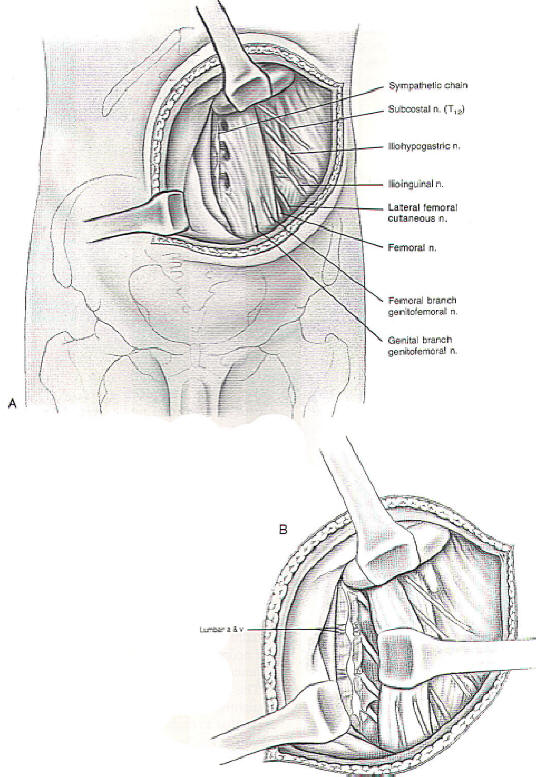
 Anterolateral Extraperitoneal Approach
Anterolateral Extraperitoneal Approach
The
anterolateral extraperitoneal approach to the upper lumbar spine
is essentially the same approach used by surgeons to gain access
to the sympathetic chain in the lumbar paravertebral region (see
Figure 4). This exposure (Figure 7) allows access to the L3-5
nerve roots from their exit point from the spinal canal to below
the pelvic brim (although with greater difficulty, the upper
lumbar nerve roots may be exposed). The patient is positioned so
that the lumbar region is extended with a log roll and the
patient rotated away from the side of the exposure. The incision
courses from the lateral half of the twelfth rib in an anterior
and medial direction. It is extended to below the level of the
umbilicus, just lateral to midline and medial to the anterior
superior iliac spine. Retraction is maintained with
self-retaining and hand-held retractors. Retraction always
should be performed with blunt instruments.
The
dissection proceeds in an anatomic manner by muscle-splitting
incisions through the external oblique, internal oblique, and
transversalis muscles along the muscle fibers of each muscle
layer. It must be kept in mind that as each anatomic layer is
passed, the surgical field becomes smaller; therefore, the
incision through each of the planes (especially the more
superficial planes) should be longer than one might expect so
that an adequate field of exposure is available when
encountering the deep structures of concern. If exposure is of
utmost importance, the internal oblique and transversus
abdominus muscles may be incised across their muscle fibers in
the same oblique direction as the skin incision.
Following
the entrance into the extraperitoneal space, the peritoneal
contents are mobilized medially with the dissection remaining
medial and posterior to the peritoneum and the renal fascia.
Finger dissection or a sponge stick may be used to sweep the
tissues away from the quadratus lumborum muscle, psoas muscle,
and vertebral bodies. The lumbar veins and arteries may be
obstacles to very medial dissection in the region of the
neuroforamina. Their ligation may be necessary for adequate
exposure. The preoperative performance of a spinal angiogram, in
these circumstances, may be prudent. The sacrifice of an
important spinal radiculomedullary artery could be catastrophic.
If high
lumbar exposure is necessary, the diaphragmatic crus may be
separated from the anterior longitudinal ligament of the
vertebral column. The sympathetic chain can be visualized in the
groove between the psoas muscle and the vertebral body. The
upper branches of the lumbosacral plexus can be visualized as
they emerge from underneath or through the psoas muscle. The
main branch of the lumbar plexus, the femoral nerve, rests
between the psoas and iliacus muscle as it courses toward the
pelvic floor. A number of the upper branches of the lumbar
plexus also can be visualized in this region. These include the
lateral femoral cutaneous. iliohypogastric, ilioinguinal and
genitofemoral nerves. The latter nerve is observed as it emerges
medially through the psoas muscle belly. The lateral femoral
cutaneous, iliohypogastric, and ilioinguinal nerves emerge
either through the lateral aspect of or from underneath (and
lateral to) the psoas muscle belly. These nerves may be followed
proximally through the psoas muscle belly to the neuroforamina
if necessary. Distal exposure is limited through this approach.
The advantages of this approach include the straightforward
nature of the exposure, which is familiar to most spine and
vascular surgeons; however, it offers a disappointingly narrow
longitudinal exposure. This exposure is limited superiorly by
the crus of the diaphragm and inferiorly by the pelvic brim.
Through this approach, it is also difficult to expose the
neuroforamina without psoas muscle retraction (which is
difficult) or resection.
|
 |
| Fig-7 |
|
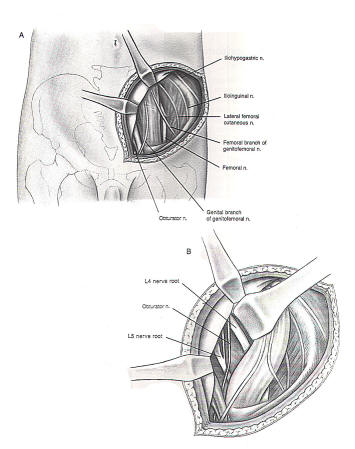
 Pelvic Brim
Extraperitoneal Approach
Pelvic Brim
Extraperitoneal Approach
The
approach to the intrapelvic portion of the lumbosacral plexus is
challenging. As for most of the techniques already described,
the exposure is defined in the spine literature for approaches
to the spine and is adapted for exposure of the lumbosacral
plexus (Figure
8). The patient
is positioned in an extended position with the log roll placed
under the lower lumbar region on the side of surgery. This
extends the lumbopelvic region and thrusts the anterior pelvic
brim on the affected side forward. It therefore increases the
visualization gained by the exposure and places the lumbosacral
plexus in closer proximity to the surgeon. An incision beginning
lateral to and slightly above the anterior superior iliac spine
can be carried medially and inferiorly, and parallel and
cephalad to the iliac crest and inguinal ligament. This gains
access to the muscular plane below this level. An incision along
the external oblique muscle fibers and across the internal
oblique and transversus abdominus muscle fibers, in turn, gains
access to the extraperitoneal pelvic structures.
Extraperitoneal structures are swept from the pelvic floor
posterior to the peritoneum and renal fascia. The nerves of the
lumbar plexus are observed emerging from between the psoas and
iliacus muscles (lateral femoral cutaneous, ilioinguinal,
iliohypogastric, and femoral nerves) and medial to the psoas
muscle (genitofemoral and obturator nerves). The obturator nerve
may be located distally by palpation at its point of exit from
the pelvis through the obturator foramen and more proximally by
medial retraction of the iliac vessels. The proximal sacral
plexus (i.e. L4 and L5 nerve root contributions) may be
visualized following lateral psoas muscle retraction and medial
iliac vessel retraction. More superficially and laterally, the
lateral femoral cutaneous nerve may be visualized. Exposure of
this nerve in this region may be required for the surgical
treatment of meralgia paresthetica.
The
advantages of this approach include the relatively good exposure
of the intrapelvic lumbar plexus from an anterior and lateral
orientation. On the other hand, it offers a limited overall
exposure, and the intrapelvic sciatic nerve and lower sacral
plexus are difficult, if not impossible, to adequately visualize
through this approach.
|
 |
|
Fig-8 |
|
 Pfannenstiel Infraperitoneal Approach
Pfannenstiel Infraperitoneal Approach
The
Pfannenstiel approach gains access to the lower pelvic
lumbosacral plexus as the femoral, obturator, and sciatic nerves
exit from the pelvis. The approach is illustrated in Figure 9.
It is a very demanding approach with limited exposure often
realized. An 8 cm horizontal paramedian excision is made in the
suprapubic region. It starts at the midline and extends
laterally. The lateral aspect of the rectus abdominus muscle is
isolated through a ventral incision in the sheath of the rectus.
The rectus abdominus muscle is retracted medially. The posterior
aspect of its sheath is then incised. This incision is extended
laterally, gaining access to infraperitoneal structures. The
sweeping of the soft tissues of the lower pelvis is performed in
a similar manner as previously described with blunt retractors
used to assist in obtaining and maintaining the exposure. Care
is taken to protect the ureter and bladder. Obviously the
bladder needs to be decompressed with a Foley catheter prior to
this surgical procedure in order to facilitate exposure.
Similarly, complete muscular relaxation is mandatory. The
sciatic nerve, as it exits the pelvis, can be isolated
underneath the psoas muscle (psoas muscle resection may be
required as discussed in the previous section). The femoral
nerve, likewise, is visualized as it rests between the psoas and
iliacus muscles. The obturator nerve can be visualized as it
passes toward the obturator foramen medial to the psoas muscle
and lateral to the iliac vessels, through this exposure.
Primary
nerve repair of branches of the lumbar plexus is difficult and
the sacral plexus impossible in this region because of the
limited and deep exposure. Ablative procedures, such as
obturator and femoral nerve neurectomies, as well as the
resection of nerve sheath tumors, however, are reasonably
approached through this exposure.
This
approach offers access to the deep pelvic paramedian structures.
Its disadvantages are obviously the degree of difficulty
associated with this exposure and the limited visualization
gained. The farther one delves into the lower limits of this
exposure, the greater the demands on the surgeon become.
|
 |
|
Fig-9 |
|
 Transperitoneal Approach
Transperitoneal Approach
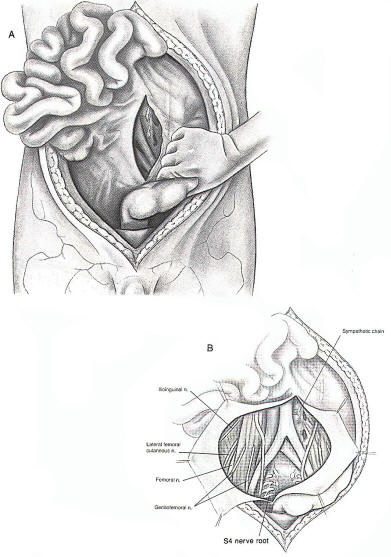
Much of the
exposure achieved by the previous three techniques may be
realized via the transperitoneal approach (Figure 10). Following
the performance of a standard midline laparatomy incision and
entry into the peritoneal cavity, the small intestine is packed
in the upper abdomen and retracted to the right. The sigmoid
colon is retracted laterally and a longitudinal incision is made
in the posterior peritoneum in the midline so as to expose the
desired aspect of the retroperitoneal space. Occasionally the
left nerve roots cannot be seen easily in this manner, and the
colon may be retracted medially and mobilized from left to right
after incision along the line of Toldt. Care should be taken to
avoid injury to the ureters.
A
horizontal low abdominal incision also may be used. This
incision extends from just medial to one anterior superior iliac
spine to just medial to the other. This incision should arc
slightly inferiorly and then rise to its terminus on the
opposite side (concave cephalad). The rectus abdominus muscles
are transected transversely. This incision may give a slightly
wider exposure to caudal structures. The sacral promontory is a
consistent, easily identifiable landmark that should be used to
identify the L5-S1 interspace.
An
excellent exposure of the retroperitoneal space is achieved
through the transperitoneal approach. Lower retroperitoneal
structures are more accessible than the more proximal
structures (especially those on the right due to the
limitations created by the presence of the sigmoid colon), such
as the proximal ilioinguinal, iliohypogastric, or genitofemoral
nerves. The disadvantages include the requirement for a
laparotomy and the potential for neural and vascular injury. The
approach, however, is very useful when a wide exposure is needed
such as for tumors of neural origin.
|
 |
|
Fig-10 |
|
 Extrapelvic
Infragluteal Approach
Extrapelvic
Infragluteal Approach
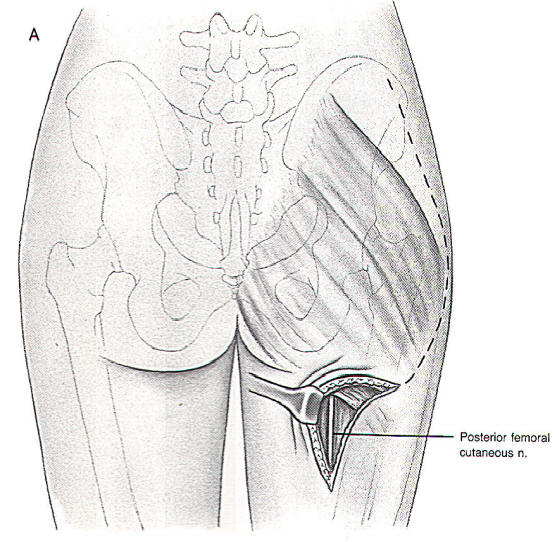
The
extrapelvic proximal sciatic nerve can be approached easily
utilizing the surgical exposure illustrated in Figure 11. The
patient is placed in the prone, semi-flexed position. A question
mark or reversed question mark incision along the lateral aspect
of the gluteus maximus muscle is made, is extended to midline
underneath the inferior aspect of the muscle, and then is
extended distally along the posterior midline of the thigh (as
dictated by the length of exposure of the nerve required. The
skin and gluteus muscles (gluteal lid) are then elevated as a
unit (without separating the skin from the gluteus muscles). In
order to elevate the flap, the gluteus muscle attachments to the
femur must be incised. This incision is performed close to the
femur itself, leaving enough length of the ligamentous
attachments to the bone so that closure is facilitated. The
extent of the reflection of the gluteus muscles from their femur
attachments is again dictated by the proximal extent of the
lesion being approached. The sciatic nerve lies deeply within
the folds between the hamstring muscles. After the isolation of
the nerve, the nerve is followed proximally. This is assisted
greatly by the reflection of the gluteal lid medially. The nerve
is followed proximally, with care taken to avoid injury to the
inferior gluteal artery. This can result not only in ischemic
complications but can be an extremely annoying intraoperative
problem. This nerve is then followed as it passes under the
piriformis muscle. The muscle may be incised to gain additional
cephalad exposure. The surgeon must be aware that the nerve may
pass through the piriformis muscle. Further dissection
immediately dorsal and adjacent to the nerve can expose the
nerve more proximally as it passes into the pelvis.
The
cephalad portion of the sciatic nerve is extremely difficult to
expose for nerve repair purposes. Surgical treatment of the
piriformis syndrome, sciatic nerve entrapment, tumors, and nerve
repair, is facilitated by this approach. A combined approach for
tumor resection at the superior extent of exposure of this
procedure and the inferior extent of the exposure from the
Pfannenstiel infraperitoneal or the anterior transabdominal
laparotomy exposure will allow access to most lesions in this
region (see next section). The advantages of this approach are
its wide exposure of the proximal extrapelvic sciatic nerve.
Proximal to the piriformis muscle, however, the exposure is
prohibitively difficult.
|
 |
|
Fig-11 |
 Combined
Approaches
Combined
Approaches
The
combined approach using the Pfannenstiel infraperitoneal and the
extrapelvic infragluteal approaches can be used to gain access
to the "relative no-man's-land" existing in the lower pelvis.
This requires, however, two different surgical procedures and
two different patient positionings; therefore, simultaneous
exposure cannot be entertained. Obviously, this is associated
with significant problems if, for example, the pull-through of a
nerve graft is desired, This should rarely, if ever, be required
because primary nerve anastomoses or cable graft anastomoses for
the proximal sciatic nerve are associated with a very low
success rate. This, therefore, leaves only tumor resection,
ablative procedures, and neurolysis procedures as indications
for exposure of this relatively difficult-to-expose area of the
nervous system.
The
Pfannenstiel infraperitoneal and the pelvic brim extraperitoneal
approaches can be used in combination and at the same time in
order to gain access to deep pelvic lesions. The exposure in
this region, although not as difficult as the exit zone of the
sciatic nerve from the pelvis, is nevertheless challenging.
Fortunately, exposure of the nerves in this region is limited
almost solely to neurolysis procedures, tumor resections, and
ablative procedures.
The
combination of the anterolateral extraperitoneal and the
pelvic brim extraperitoneal approaches would be appropriate
for pathology traversing the boundaries of these two
surgical approaches. The longitudinal exposure obtainable
with the combination of these approaches is substantial.
Such an extensive exposure, however, seldom would be
necessary.
Similarly, the overlap between the proximal exposure of the
anterolateral approach and the lateral extracavitary
approach is extensive. A combination of these two
approaches, therefore, seldom would be indicated. This is
especially fortunate since two separate incisions with two
separate surgical positionings would be required (as is the
case with the extrapelvic infragluteal and Pfannenstiel
infraperitoneal approaches).
For
proximal lesions (especially those involving the spinal
canal or intradural structures), a combined approach using
the wide foraminotomy and the lateral extracavitary
approaches is indicated. The combination of these two
approaches is easily facilitated by the flap incision or
perhaps, more appropriately, by a paramedian vertical
incision. The paramedian vertical incision diminishes the
chance of skin-flap vascular complications and healing
problems while allowing ready access to both regions.
Another advantage of the combined approach is that the facet
joint usually can be left intact if an aggressive distal
exposure via the lateral extracavitary approach and a
proximal exposure via a wide foraminotomy are performed.
The
transperitoneal approach alone offers a wide anterior
midline exposure as well as many of the advantages of some
of the combined approaches mentioned previously. If the
risks associated with this technique offset the combined
risks of the two or more individual approaches used in a
combined approach, then the transperitoneal approach may be
the best option.
 Complications
Complications
The
complications that may be encountered during or following
the surgical approaches to the lumbosacral plexus are
numerous. Perforation of the vena cava, aorta, iliac
vessels, or lumbar arteries and veins may be catastrophic
or, at the very least, a significant nuisance. Singultus
secondary to intraoperative diaphragm manipulation may be
disconcerting to both the patient and physician. Similarly,
wound dehiscence or hernia may cause significant morbidity.
Retroperitoneal dissection may result in disruption of vital
structures located in this space, such as vascular
structures (as mentioned before) and urogenital structures.
A knowledge of the whereabouts of important structures, such
as the ureter, is of paramount importance during exposure of
anatomic regions where these structures may be injured. In
cases where the dissection is complicated by extenuating
factors, such as prior radiation therapy, surgery, or
extensive tumor bulk, the preoperative placement of a
ureteral stint by an urologist may allow the intraoperative
identification of the ureter. This may prevent a potentially
catastrophic ureteral injury.
Finally,
injury to radiculomedullary spinal arteries may result in
paraplegia. Appropriate diagnostic avenues (such as angiography)
must be used when such an injury may result from the surgical
exposure. Alterations of surgical technique must be entertained
if angiography demonstrates the presence of a radiculomedullary
spinal artery in the region of planned dissection.
|