|
In this section
the emphasis is directed to other entrapment
syndromes.
 Etiology
Etiology
The compressed segment is in a
specific location on the nerve as determined by the
local anatomy, i.e. where the nerve traverses a
tunnel bound by bone and fibrous tissue or where the
nerve passes from one compartment to another.
Changes in the tissue consistency that surrounds the
nerve can precipitate entrapment. Trauma with direct
injury or callus formation after fracture also has
been implicated. Systemic diseases that have been
associated with entrapment include hypothyroidism,
acromegaly, rheumatoid arthritis, osteoarthritis,
giant-cell arteritis, and amyloidosis. An anatomic
variant, such as an accessory muscle, arterial
aneurysm, or congenitally small tunnel, can
precipitate an entrapment neuropathy as well.
Compression of the posterior interosseous nerve, for
example, has been described with hemihypertrophy and
with a lipoma in the region of the elbow. There are
cases with compression of the median nerve by a
lipoma in the deep palmar space and compression of
the ulnar nerve by a schwannoma in the cubital
tunnel.
Occupational causes of neuropathy are
common. Carpal tunnel syndrome has been reported as
an overuse syndrome in persons who employ sign
language for the deaf. The carpal tunnel syndrome
has been observed in patients with paraparesis who
use crutches for walking. Compression of the ulnar
nerve in Guyon's canal is seen in cyclists.
Compression of the ulnar nerve is legendary in
patients who spend long hours leaning their elbows
on bars.
The probable cause of entrapment
neuropathy is a decrease in the neural blood supply.
The nerve receives its blood supply from the
mesoneurium, which is flexible and permits
continuing perfusion as the extremity moves. Venous
obstruction caused by compression increases
intrafascicular pressure. This, in turn, decreases
perfusion, which leads to edema. A vicious cycle
ensues. An ingrowth of fibroblasts and scar
ultimately results. This adds to the vicious cycle
of worsening hypoxia. Diabetes, which compromises
the blood supply, places the nerve at an additional
risk of compression and repetitive injury.
Compression and atrophy can be so long-standing that
end organ fibrosis may result. In this situation,
decompression of the nerve will not improve the
neurologic symptoms.
The electrodiagnostic findings in any
entrapment neuropathy depend on a number of
variables including (1) the timing of the study, (2)
the severity of the injury, and particularly (3) the
relative amounts of demyelination and axonal loss.
In the experience of a competent
electrodiagnostician, normal findings are rarely
identified as abnormal. Conversely,
electrodiagnostic evaluations may be inadequate to
identify minor injuries to nerves. This situation
can occur in proximal demyelinating lesions when
conduction studies cannot be obtained above and
below the suspected lesion due to technical
limitations. In addition, false-negative results or
inconclusive results may occur because of premature
testing. Complete expression of an abnormality may
require up to 7 days for motor nerve conduction. 9-
10 days for sensory conduction, and 3 weeks for
needle examination of muscle; however,
electrodiagnostic studies are useful to diagnose
other syndromes, such as proximal lesions, multiple
lesions, or lesions that accompany diabetes
mellitus.
 Differential
Diagnosis
Differential
Diagnosis
Strict criteria should be used to
diagnose entrapment neuropathies. It is regular to
see patients with spondylotic myelopathy and
radiculopathy who have undergone unnecessary carpal
tunnel surgery. The peak age for both conditions is
the same, and many of these patients have electrical
evidence of carpal tunnel syndrome.
Radiculopathy involving the C8 nerve
root can be confused with ulnar neuropathy. When the
patient has thenar atrophy as well as involvement of
the ulnar nerve, a C8 nerve root lesion should be
suspected strongly. A double crush syndrome is when
cervical or thoracic outlet compression worsens
median or ulnar entrapment. It is unusual for a
patient to have more than one lesion. A high index
of suspicion, the unique symptoms and physical
findings, the results of electrodiagnostic studies,
and, when necessary, cervical spine imaging should
lead to the correct diagnosis.
 Internal Neurolysis
Internal Neurolysis
The value of internal neurolysis at
the time of decompression has long been debated.
Mackinnon and colleagues documented an improved
electrical and morphologic recovery with neurolysis
compared to decompression alone in a rat model. In a
clinical paper, however, Mackinnon and colleagues
demonstrated that although neurolysis is a safe
procedure, it does not provide clinical benefit in
patients who have had carpal tunnel surgery.
Neurolysis of a nerve whose diameter is diminished
by a circumferentially thickened and scarred
epineurium may improve nutrition and permit nerve
expansion during healing. Nevertheless, neurolysis
is not necessary for all patients undergoing carpal
tunnel surgery or with compressed nerves.
Performance of internal neurolysis in every carpal
tunnel operation courts disaster. The decision on
whether or not to perform a neurolysis depends on
the observation of the nerve in the operating room.
If the nerve remains narrowed after the surgical
decompression or if intraneural scarring is present,
neurolysis should be done. Patients who present with
recurrent symptoms could have neurolysis. After
neurolysis, the fascicles, even if atrophic, will be
obvious and not hidden in thick epineurium.
 Median Nerve
Median Nerve
The more proximal median compression
syndromes can produce pain, neurologic deficit, or
both. The compression can occur above the elbow at
the ligament of Struthers or below the elbow by the
pronator teres muscle (Figure 1A,B,C).
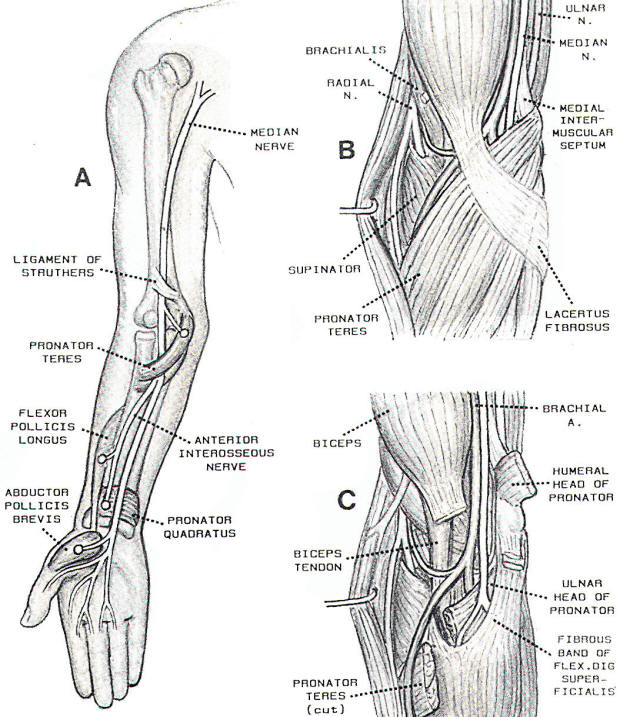
Fig-1
 Entrapment at
Ligament of Struthers
Entrapment at
Ligament of Struthers
The ligament of Struthers, which
should not be confused with the arcade of Struthers
(which produces ulnar neuropathy), is located 5 cm
proximal to the medial epicondyle. The median nerve
and brachial artery both pass beneath this ligament.
Nerve compression at the ligament of Struthers
usually produces a syndrome of pain and local
tenderness. The anterior interosseous nerve branch
of the median nerve can be compressed at the
ligament of Struthers, with resultant motor
neuropathy. This phenomenon is unusual. The
electrodiagnostic findings demonstrate a reduced or
absent median sensory potential. With a
predominantly demyelinating lesion, conduction
velocity may be slowed across the involved segment
with a normal conduction velocity below. Conduction
study motor amplitudes will be reduced after axon
loss, regardless of the site of stimulation. With
demyelination, however, motor amplitudes are
abnormal only with stimulation above the site of the
lesion. With any amount of axon loss, denervation
will be evident in all median innervated muscles of
the hand and forearm. Section of the ligament
effectively relieves symptoms.
 Pronator Syndrome
Pronator Syndrome
The pronator syndrome is
characterized by mild to moderate pain in the
forearm. The pain increases with movement of the
elbow, with repeated supination and pronation,
and with repeated use of the grip. Loss of
dexterity in the hand, mild weakness, and median
nerve paresthesia occur. Numbness may be
present, not only in the fingers, but also in
the thenar region of the palm because of
involvement of the palmar cutaneous nerve that
branches distal to the site of compression.
These symptoms resemble carpal tunnel syndrome,
but the symptoms of paresthesia while sleeping
are absent. The pain in the forearm and the
local tenderness can be reproduced by resisted
pronation. Tinel's sign may be present over the
nerve.
The anatomic level of compression
is within the substance of the pronator teres
muscle. The median nerve with the brachial
artery lies between the two heads of the
pronator teres and passes deep to the fibrous
origin of the flexor digitorum superficialis
muscle. Compression may be caused by the
thickened lacertus fibrosus, by a hypertrophied
pronator muscle, or by a tight fibrous band of
the flexor digitorum superficialis muscle.
Results of electrodiagnostic studies are often
normal. When results are abnormal, they parallel
the findings in patients with the ligament of
Struthers syndrome except that no denervation is
present in the pronator teres muscle.
Treatment of patients with the
pronator syndrome is initially conservative with
administration of anti-inflammatory medication
and use of splints. An attempt is made to
eliminate precipitating events. Should these
measures be ineffective, surgery should provide
good results. The lacertus fibrosus is released
and the median nerve is translocated to a
subcutaneous position anterior to the pronator
teres muscle. The nerve should be exposed from
the distal upper arm to the middle forearm. The
median nerve and its major branches should be
visualized. Care should be taken to preserve the
branches of the medial cutaneous nerve of the
forearm. Injury to this nerve can produce a
painful neuroma.
 Anterior
Interosseous Nerve Syndrome
Anterior
Interosseous Nerve Syndrome
The anterior interosseous nerve
separates from the main median nerve
approximately 8 cm distal to the lateral
epicondyle. It gives off a sensory branch to the
wrist joint and provides motor innervation to
the flexor pollicis longus muscle, the flexor
digitorum profundus muscle of the index and
middle fingers, and the pronator quadratus
muscles. The site of compression is slightly
more distal in the mass of the pronator teres
muscle than that for the pronator syndrome. The
compression is caused by the tendinous origin of
the deep head of the pronator teres muscle,
which crosses the anterior interosseous nerve at
its origin from the parent median nerve. An
enlarged bicipital bursa has also been described
as the causative agent. Whereas pain and
tenderness are present in the forearm of
patients with the anterior interosseous nerve
syndrome, the predominant symptoms and objective
findings are motor. When untreated, the pain
often resolves. Motor loss then follows.
Characteristically, an abnormal pinch is
produced because of the inability to flex the
interphalangeal joint of the thumb.
Results of nerve conduction
studies typically are normal in patients with
the anterior interosseous nerve syndrome.
Results of needle electromyography indicate
denervation restricted to the three muscles
innervated by the nerve. Occasional patients may
present clinically with the anterior
interosseous nerve syndrome and with
electrodiagnostic proof of a more proximal
lesion of the median nerve. Presumably, the
fascicles destined to become the anterior
interosseous nerve are affected more selectively
in this situation. The surgical exposure for
patients with this syndrome is similar to that
described for the pronator syndrome.
 Ulnar Nerve
Ulnar Nerve
In addition to the ulnar nerve
compression found at the cubital tunnel, ulnar
neuropathies can be caused by compression at the
arcade of Struthers and in Guyon's canal.
Because the sensory symptoms are located on the
medial aspect of the hand and arm, it is
necessary to be certain that the condition is
not caused by a C8 nerve root or lower brachial
plexus lesion.
 Arcade of
Struthers
Arcade of
Struthers
The arcade of Struthers (Figure
2A) is located where the ulnar nerve passes
through the medial intermuscular septum into the
posterior compartment. The arcade is a fibrous
septum that is located 8 cm proximal to the
medial epicondyle. It is present in only 70% of
patients. The arcade of Struthers is rarely a
site of primary compression. It may, however,
become important following an anterior
transposition of the nerve as a proximal tether
impinging on the nerve. It is important to
release the band when transposing the nerve to
prevent this secondary compression.
 Guyon's Canal
Guyon's Canal
Guyon's canal is found on the
medial aspect of the wrist (Figure 2B). The
anterior border of Guyon's canal is the volar
carpal ligament, whereas the posterior border is
the transverse carpal ligament. Within the
canal, the ulnar nerve runs with the ulnar
artery and vein and divides into motor and
sensory branches. The distal lesion affects only
the motor branch, and the more proximal lesion
affects both the motor and the sensory branch.
Because the motor branch is deeply placed and
tethered as it passes around the hook of the
hamate bone, it is prone to compressive lesions.
Spaceoccupying lesions, such as ganglia,
produce compression as does chronic occupational
trauma in cyclists and in persons who use their
hands as hammers. Space-occupying lesions may be
encountered in patients with fracture of the
pisiform bone or hook of the hamate bone.
Pure motor paresis produces a
claw hand as a result of intrinsic weakness and
separation of the fourth and fifth fingers
(Wartenberg's sign). Mixed nerve compression
produces paresthesia and sensory loss as well as
the typical clawhand.
Electrodiagnostic findings again
depend on whether the lesion is predominantly
axonal or demyelinating. With demyelinating
lesions, slowing of motor and sensory latencies
across the wrist may be expected, particularly
when sensory studies are performed by the palmar
technique, and the motor conductions are
performed while recording from the first dorsal
interosseous muscle. In axonal lesions, motor
and sensory amplitudes are reduced and
denervation is found in the ulnar muscles of the
hand. Reduced amplitude of the dorsal cutaneous
branch of the ulnar nerve or denervation in the
ulnar muscles of the forearm implies the
existence of a lesion proximal to the wrist.
When the patient's condition does
not respond to the use of splints and the
administration of anti-inflammatory medications,
the canal should be explored. Surgery in this
instance usually is indicated earlier than in
patients with other compression neuropathies
because of the motor involvement. Both
superficial and deep branches of the nerve
within the canal should be explored carefully.
Any mass within the canal, such as a ganglion
cyst or a displaced hook of the hamate bone,
should be removed.
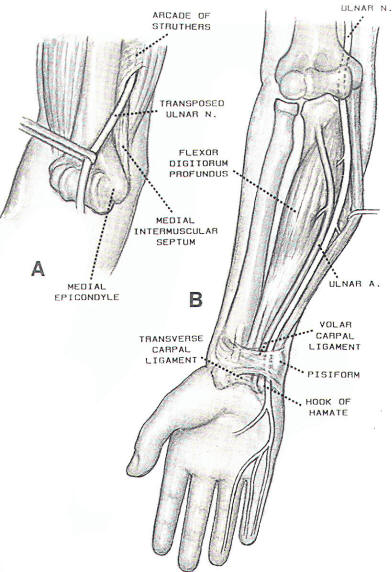
Fig-2:
 Radial Nerve
Radial Nerve
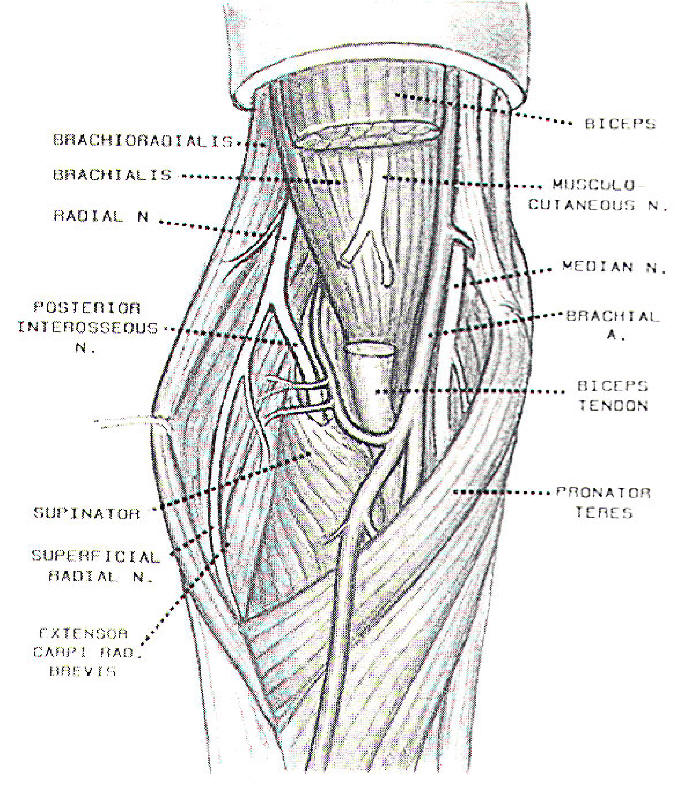
Compression neuropathies of the
radial nerve produce clinical syndromes dependent on
the level of compression (Figures 3 and 4). The
lesion in the proximal arm is rarely spontaneous but
is associated with trauma, most commonly fracture of
the humerus. "Saturday night palsy" results from
compression of the radial nerve when the patient
sleeps heavily with the posterior arm resting
against a firm edge. The patient presents with
wristdrop and an inability to extend the fingers.
This condition usually is associated with sensory
loss because of the high level of the nerve injury.
Of patients who present with radial nerve palsy. 80%
recover spontaneously; therefore, exploration is not
performed early in most instances. If the palsy is
associated with fracture of the humerus, however,
early surgery may be appropriate. When the nerve is
explored, it should be freed from the bone fragments
or callus and reanastomosed when divided.
In patients with demyelinating
lesions of the radial nerve at the middle to
proximal humerus, results of conduction studies
distal to the lesion are normal. Studies performed
proximal to the lesion will show a reduced or slowed
motor response compared with stimulation distal to
the lesion. In patients with axonal lesions, radial
motor and sensory amplitudes are reduced and
denervation is found in all radial muscles
innervated distal to the triceps muscle. Changes on
electromyography are not observed until 3 weeks
after the injury.
The radial nerve curves around the
posterior humerus in the spiral groove and enters
the anterior aspect of the arm, 10 cm proximal to
the lateral epicondyle, by passing through the
lateral intermuscular septum. The radial nerve
passes anterior to the radiohumeral joint where it
divides into superficial and deep branches. The
superficial branch proceeds distally, deep to the
brachioradialis muscle, to provide sensation to the
dorsum of the first web space in the hand. The deep
branch spirals around the neck of the radius,
passing between the two heads of the supinator
muscle, to enter the posterior aspect of the arm as
the posterior interosseous nerve (Figure 4A). The
deep branch supplies the extensor muscles of the
wrist, hand, and thumb except for the extensor carpi
radialis longus muscle, which is innervated by a
branch from the radial nerve before it enters the
supinator muscle.
 |
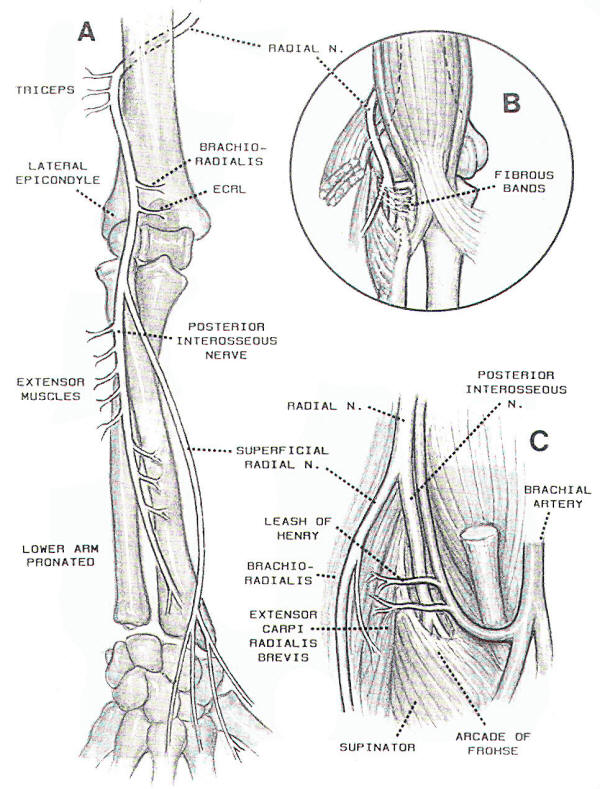 |
| Fig-3 |
Fig-4 |
 Radial Tunnel
Syndrome
Radial Tunnel
Syndrome
The clinical syndrome associated with
compression of the deep branch of the radial nerve
has been called the radial tunnel syndrome. It may
be confused with tennis elbow. The radial tunnel
syndrome, however, produces a deep somatic ache in
the extensor muscles, usually exacerbated by
exercise, without sensory or motor symptoms. Four
potential sites of compression exist: (1) by fibrous
bands anterior to the radial head (Figure 4B), (2)
by vessels of the leash of Henry that pass over the
radial nerve to supply the brachioradialis muscle,
(3) by the tendinous margin of the extensor carpi
radialis brevis muscle, and (4) by the arcade of
Frohse, which is the sharp ligamentous margin of the
superficial head of the supinator muscle (Figure
4C). The latter is the most common site of
compression. This sharp edge is not present in the
fetus. It is fibrotendinous in 30% of limbs. The
arcade of Frohse forms in response to repeated
rotary movements of the arm. This syndrome in the
dominant arm in 89% of patients. Most patients have
a history of repetitive trauma, such as is observed
in bricklayers, pipe fitters, machine operators,
orchestra conductors, and tennis players. Other
causes of compression may be tumor, lipoma, synovial
proliferation in rheumatoid arthritis, or fracture
of the head of the radius.
 Tennis Elbow
Tennis Elbow
In discussing the broad diagnosis of
tennis elbow, a range of disorders from lateral
epicondylitis to severe extensor weakness, they
included the radial tunnel syndrome. On examination,
tenderness is present over the lateral epicondyle of
the humerus or just distal to the radial head where
the nerve travels into the supinator muscle. A
typical increase in pain occurs when extension of
the middle finger is resisted. This maneuver will
tighten the origins of the extensor carpi radialis
brevis muscle and further compress the nerve. Injury
to the origin of the extensor carpi radialis brevis
tendon at the lateral epicondyle is related to
epicondylitis-the classic tennis elbow. Local
injection with lidocaine and a corticosteroid
provides only temporary relief of symptoms.
Results of electrodiagnostic studies
may demonstrate delays in motor latencies from the
spiral groove to the medial border of the extensor
digitorum communis muscle, but they are frequently
normal. For patients whose neuropathy does not
respond to avoidance of trauma, use of splints, and
administration of anti-inflammatory medications,
surgical exploration with decompression of the
superficial radial nerve is indicated.
 Posterior
Interosseous Nerve Syndrome
Posterior
Interosseous Nerve Syndrome
The syndrome of the posterior
interosseous nerve differs from the radial tunnel
syndrome in that the predominant symptoms and
findings are motor rather than pain or sensory loss.
The arcade of Frohse is the major constricting
structure. Severe weakness of the radial innervated
muscles exists with inability to extend the fingers
at the metacarpophalangeal joint. The wrist
dorsiflexes in a dorsoradial direction because of
paralysis of the extensor carpi ulnaris and the
extensor digitorum communis muscles. The
brachioradialis, extensor carpi radialis longus,
extensor carpi radialis brevis, and supinator
muscles are not weak because these muscles are
innervated by branches that arise before the point
at which the radial nerve enters the arcade of
Frohse. In this syndrome, pain and local tenderness
are followed by progressive motor loss. When sensory
loss is present, a more proximal lesion must be
considered.
The electrodiagnostic findings of an
axonal injury to the posterior interosseous nerve
consist of normal radial sensory studies. Normal or
reduced amplitude of the radial motor response
occurs when recording from a distal radial nerve
innervated muscle. Denervation will be found in all
radial nerve innervated muscles excluding the
triceps, brachioradialis, extensor carpi radialis
longus, extensor carpi radialis brevis, and anconeus
muscles.
For patients with the posterior
interosseous nerve syndrome with significant motor
findings, surgical exploration is indicated. For
patients with a less severe clinical course, rest,
the use of splints, and the administration of
anti-inflammatory medications are indicated.
 Wartenberg's Syndrome
Wartenberg's Syndrome
Wartenberg's syndrome is a rare
syndrome that results from the compression of the
superficial radial nerve in the forearm. This
syndrome is characterized by pain in the proximal
forearm and hypoesthesia over the dorsal thumb. No
weakness is present. The compression is usually
caused by trauma or wearing a tight band or watch.
Electrodiagnostic findings of a superficial radial
neuropathy consist solely of a diminished or absent
radial nerve sensory response.
|
 Suprascapular Nerve Entrapment
Neuropathy
Suprascapular Nerve Entrapment
Neuropathy
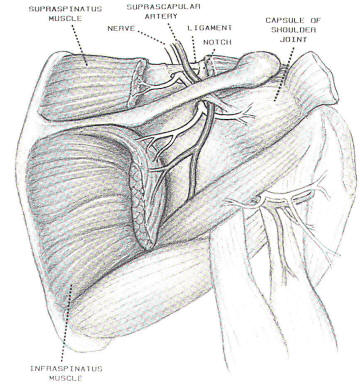
The suprascapular nerve
is a mixed peripheral nerve that
provides motor innervation to the
supraspinatus and infraspinatus muscles
(Figure 5). The nerve has no cutaneous
distribution but provides sensory supply
to the posterior capsule of the shoulder
joint. The syndrome of suprascapular
nerve compression includes aching in the
posterior aspect of the shoulder with
weakness and ultimately atrophy of the
muscles involved. Weakness and atrophy
produce difficulty in lifting the arm
overhead and weakness of external
rotation. Wasting of the infraspinatus
muscle is obvious because less tissue
overlies the infraspinatus muscle. The
lack of involvement of the deltoid and
rhomboid muscles differentiates this
lesion from a C5 nerve root lesion.
nerve. The
suprascapular nerve begins as a branch
from the upper trunk of the brachial
plexus and runs parallel and lies deep
to the inferior belly of the omohyoid
muscle. It travels deep to the trapezius
muscle and through the suprascapular
notch into the supraspinous fossa. In
the notch the suprascapular ligament
compresses the |
 |
|
Fig-5 |
|
The suprascapular artery
passes superficial to the ligament. In
the supraspinous fossa, the remainder of
the nerve curves around the lateral
margin of the spine to enter the
infraspinous fossa. The suprascapular
notch is a continuum between a widely
patent notch and a bony foramen. The
smaller notch is more likely to be
involved with entrapment neuropathy. The
sling effect in which the nerve is
compressed by the sharp inferior edge of
the ligament. Plain roentgenography of
the scapula, visualizing the notch, may
be helpful in establishing the
diagnosis. Repetitive trauma has been
implicated in the origin of this
neuropathy, although it is observed in
patients with isolated trauma, condition
in a person who used poorly fitted
crutches with excess shoulder depression
and an exaggerated swing.
Conduction studies of the
suprascapular nerve are not accomplished
readily. Denervation in the
supraspinatus and infraspinatus muscles,
sparing the cervical paraspinal,
deltoid, and rhomboid muscles. is
consistent with this diagnosis. Surgical
release of the nerve should be performed
early. Relief of pain is prompt, but
that motor function returns slower.
|
|
 Thoracic
Outlet Syndrome
Thoracic
Outlet Syndrome
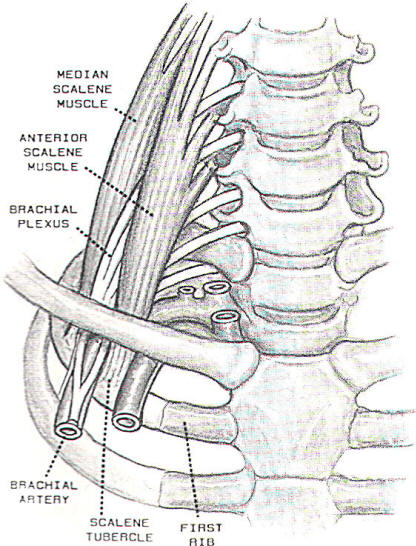
The thoracic outlet
syndrome is a controversial subject. In
some institutions, it is diagnosed and
treated so often that one would think it
constitutes a menace to public health.
In other institutions, it is rarely
diagnosed. Before the controversy is
discussed, the conventionally held views
regarding anatomy, symptoms, findings,
and treatment are described.
The brachial
neurovascular bundle goes through the
thoracic outlet to enter the arm. The
thoracic outlet is divided into the
intrascalene triangle, the
costoclavicular space, and the
subcoracoid tunnel. Most cases of
neurovascular compression occur in the
first portion by an anomalous first rib
or by fibromuscular bands running from
the tip of an incomplete rib or a
prominent C7 transverse process to the
scalene tubercle of the first rib. Other
acquired conditions that can compress
the brachial plexus should be kept in
mind, such as fracture with callus
formation, aneurysms of the subclavian
artery, and tumors (most commonly a
Pancoast tumor).
Wilbourn described five
clinical syndromes. The first is a major
arterial syndrome. This syndrome is
associated with a bony anomaly, such as
a cervical rib. The arterial wall is
damaged and poststenotic dilatation
occurs. Thrombus may be found in the
vessel, disposing to distal emboli and
Reynaud's phenomenon. This condition may
constitute a surgical emergency.
|
 |
|
Fig-6 |
|
The second is a minor
arterial syndrome. Eighty percent of
adults reduce or obliterate their radial
pulse when they elevate, abduct, and
externally rotate their arm. Using
photoplethysmography during provocative
tests in normal subjects. Considerable
but asymptomatic arterial obstruction in
60% of subjects and bilateral
obstruction in 33 % of subjects is
noted. The third is the venous
obstruction syndrome. Spontaneous
thrombosis of the subclavian or axillary
vein may be observed in young adults
after vigorous repetitive activity of
the upper extremity. Cyanosis, swelling,
and aching of the limb occur. The
brachial plexus is not involved. The
classification of this syndrome as a
type of a thoracic outlet syndrome may
not be correct.
The fourth is the true
neurogenic thoracic outlet syndrome. The
major component in this syndrome is
weakness and wasting of the intrinsic
muscles of the hand. This syndrome is
also associated with intermittent aching
in the medial forearm and is the only
widely accepted thoracic outlet
syndrome. The pathologic finding is
usually the fibrous band from a
rudimentary cervical rib to the first
rib that compresses the lower trunk of
the brachial plexus. In 75 % of
patients, all of the intrinsic muscles
are weak and wasted. The thenar muscles
are most severely wasted because the
lower trunk plexopathy most severely
affects median nerve fibers to the
thenar eminence. Rarely will a patient
with true neurogenic thoracic outlet
syndrome have reduced ulnar sensory
amplitude as well as reduced median and
ulnar motor amplitude on the affected
side. Median, ulnar, and radial nerve
innervated muscles, which are also
innervated by the lower trunk and medial
cord of the brachial plexus, will be
denervated. Treatment is surgical
removal of the offending band, The
prognosis for the wasted muscle of the
hand is poor. The last group is termed
by Wilbourn, as the "disputed neurogenic
thoracic outlet syndrome." Most
operations are performed for this group.
Wilbourn, believes that the criteria for
surgery are usually broad and poorly
defined. This pain syndrome is without
anatomic or physiologic changes. No
objective clinical or laboratory
findings exist. Results of
electrodiagnostic studies are normal. No
evidence is present to suggest that
serious neural compression will occur if
the condition is not treated. The
incidence of documented neurosis and
litigation is high in this group of
patients. A moratorium should be placed
on surgery for patients with the
disputed thoracic outlet syndrome; a
significant complication rate associated
with the operation. Postoperative
evaluations by an independent
neurologist reported persistence of
symptoms in the face of the surgeon's
report of excellent results.
In the thoracic outlet
syndrome, as well as in the other
entrapment neuropathies, careful
evaluation of the history and physical
examination and results of
electrodiagnostic studies should permit
proper selection of patients for
treatment and performance of the
appropriate surgical procedures.
|
|