|
Anamnesis
 |
The patient came to the clinic 25-February-2004
complaining of severe headache for several
months and blurred vision lat month with
anosmia. |
 |
MRI brain with contrast done 14-February-2004
showing huge olfactory groove meningioma more to
the left with massive edema over the left
cerebral hemisphere. |
 |
On examination: The patient has anosmia with
decreased visual functions more the left eye
with scatomas. She had episodes of vomiting the
last 2 weeks. The patient has epiattacks and she
felt down in the bathroom one week ago. |
 |
Modified left bifrontal
craniotomy done with reflection of the bone flap
to the left ear. The brain is severely swollen
and all measures to decrease the swelling
failed. Trying to minimize the traction injury,
the tumor was approached and piece-meal
resection was achieved. Total resection of the
mass was done, but the brain swelling persisted.
The wound was closed, so that the dura was not
pushing the brain. The patient was extubated and
sent to the ICU. The patient still drowsy and
she was sent for control CT-scan of the brain,
which revealed very huge occipital hematoma. The
patient was taken to the operating room and the
hematoma was evacuated, after what good recovery
was achieved. |
FOLLOW UP
 |
The patient had huge extradural hematoma, which
was the cause of the swelling and made the first
operation difficult. Usually after resection of
the tumor. the brain becoming lax and
regain good pulsation, but here was not the
case. |
 |
In retrospective analysis, the hematoma must be
diagnosed first and removed and then remove the
tumor. But for several reasons the hematoma was
missed and the first surgery was very difficult. |
 |
In the future do the MRI investigations
immediately before surgery. |
 |
The patient came
to the clinic
09-April-2007 to discontinue Epanutin. She is convulsion free for
three years. On examination, the right eye still having decreased
vision with bilateral anosmia. |
OLFACTORY GROOVE MENINGIOMAS
Clinical Features
These tumors arise from the midline of the anterior
fossa between the crista Galli and the tuberculum
sella. They are usually bilateral but may be asymmetric
and attain a large size before causing symptoms. The
most common presenting symptom is a subtle change in
mental function or headache alone or in combination with
mental function change, but a disturbance in vision or a
seizure disorder may also be the initial manifestation.
Loss of the sense of smell was recorded as "possibly"
the primary symptom in only 3 of 28 patients in
Cushing's series, and he questioned the reliability of
this finding.
MRI clearly defines the extent of the tumor, the edema
in the surrounding brain, the relationship of the tumor
to the optic nerves and anterior cerebral arteries, and
any extension into the ethmoid sinus. Angiography is
rarely needed.
Surgical Management
In planning the operation, it is important to remember
that the blood supply comes into the tumor through the
bone in the midline of the anterior fossa from branches
of the ethmoidal, middle meningeal, and ophthalmic
arteries; the posterior capsules may be attached to the
optic nerves, chiasm, and anterior cerebral arteries.
For patients with a large tumor, It is preferable to
perform a bifrontal craniotomy. This approach is
associated with the least amount of retraction on the
frontal lobes, gives direct access to all sides of the
tumor, and allows the surgeon to decompress the tumor
while working along the base of the skull to interrupt
the blood supply. For smaller tumors, a right subfrontal
approach coming from laterally over the orbital roof, as
for tuberculum sella meningioma, may be used. Some uses
a pterional approach. Others use either exposure and may
resects part of the frontal lobe. The patient is placed
carefully in the supine position with the head elevated
and slightly extended. Using a coronal incision, the
skin flap and underlying tissue, including pericranial
tissue, are turned down together. Burr holes are placed
just below the end of the anterior temporal line and on
each side of the saggital sinus at the level of the skin
incision. The cut just above the supraorbital ridge is
made from each side as far medially as possible. Usually
this leaves a centimeter or less of bone in the midline.
Because of the irregular bone projecting from the inner
table of the skull in this area, it is often not
possible to cut completely across the area, but the
external table can be cut with a fine drill attachment
and the bone can be broken at this point. The frontal
sinuses are almost always entered. The mucosa is removed
and the sinuses are packed with bacitracin-soaked
Gelfoam. A flap of pericranial tissue from the back of
the skin flap is turned down over the sinuses and sewn
to the adjacent dura. The dural incision is made over
each medial inferior frontal lobe just above the edge of
the craniotomy opening. While the frontal lobes are
retracted carefully, the superior sagittal sinus is
divided between two silk sutures and the falx is cut.
The frontal lobes are then retracted carefully laterally
and slightly posteriorly. The tumor will come into view
in the midline; at times it is found to have grown into
the region of the crista galli and falx. The anterior
capsule of the tumor is exposed, and then an extensive
internal decompression is done. The base of the tumor in
the midline is gradually divided, interrupting the blood
supply that is coming in through numerous openings in
the bone. These are occluded with coagulation and bone
wax. The capsule can now be reflected into the area of
the decompression without undue pressure on the frontal
lobes. Great care is taken during the dissection of the
posterior portion of the capsule. The surgeon reflects
it anteriorly and is careful to look for the
pericallosal branch of each anterior cerebral artery.
The frontal polar branch will often be adherent to the
tumor and may need to be divided. It is usually possible
to follow the capsule back to the sphenoid wing and
then, working medially, to identify the anterior clinoid
processes and the optic nerves. At times it may be
difficult to see the nerves because of the posterior and
inferior compression and the thickened arachnoid.
However, under magnification, the tumor can be reflected
off the optic nerve(s). Once the bulk of the tumor is
removed, the dural attachment is totally excised and any
bone hyperostosis removed, with care taken to avoid
entering the ethmoid sinus unless it is known that the
tumor extends into the sinus. The region of the
cribriform plate is covered with a graft of pericranial
tissue and Gelfoam to prevent a cerebrospinal fluid
(CSF) leak.
Results
Complete removal can be achieved in 90% of cases and 5%
with a radical subtotal removal with a small fragment
left on the internal carotid artery or other vitally
important structures. In 90% of patients a good result
can be achieved. Postoperative death due to various
causes is around 5%.
The incidence of complications is low and do not
interfere with eventual recovery. CSF leak through the
ethmoid sinus that required transethmoidal repair can be
in 5% of cases. A wound infection also 5%, A subdural
hygroma requiring a subdural-peritoneal shunt in 5%.
Disturbance in mental function and personality changes
when present preoperatively or transiently in the
postoperative period usually recover completely.
Preoperative visual symptoms usually recover and
headache is relieved.
Background
A systematic investigation of long-term follow-up
results after microsurgical treatment of patients
harbouring an olfactory groove meningioma, particularly
with regard to postoperative olfactory and mental
function, has rarely been performed. We reassessed a
series of patients treated microsurgically for an
olfactory groove meningioma in regard to clinical
presentation, surgical approaches and long-term
functional outcome. Method. Clinical, radiological and
surgical data in a consecutive series of 56 patients
suffering from olfactory groove meningioma were
retrospectively reviewed.
Findings. Presenting symptoms of the 41 women and 15 men
(mean age 51 years) were mental changes in 39.3%, visual
impairment in 16.1% and anosmia in 14.3% of the
patients. Preoperative neurological examination revealed
deficits in olfaction in 71.7%, mental disturbances in
55.4% and reduced vision in 21.4% of the cases. The
tumour was resected via a bifrontal craniotomy in 36, a
pterional route in 13, a unilateral frontal approach in
4 and via a supraorbital approach in 3 patients. Extent
of tumour resection according to Simpsons
classification system was grade I in 42.9% and grade II
in 57.1% of the cases. After a mean followup period of
5.6 years (range 113 years) by clinical examination and
magnetic resonance imaging (MRI), 86.8% of the patients
resumed normal life activity. Olfaction was preserved in
24.4% of patients in whom pre- and postoperative data
were available. Mental and visual disturbances improved
in 88 and 83.3% of cases, respectively. Five recurrences
(8.9%) were observed and had to be reoperated.
Conclusions
Frontal approaches allowed better resection of tumours
with gross infiltration of the anterior cranial base,
tumours extending into the ethmoids or nasal cavity and
in cases with deep olfactory grooves. Preservation of
olfaction should be attempted in patients with normal or
reduced smelling preoperatively.
Introduction
Meningiomas of the midline anterior skull base include
tumours originating from the dura of the cribriform
plate, planum sphenoidale and tuberculum sellae and
account for about 10% of all intracranial meningiomas
[41]. For clinical, radiological and surgical purposes
true olfactory groove meningiomas, i.e. tumours
originating from the dura between the crista galli and
the frontosphenoid suture should be differentiated from
planum sphenoidale and tuberculum sellae meningiomas [8,
32]. Tumours arising from the latter sites usually come
to clinical attention at an early stage with visual
deterioration, while this is a late feature in olfactory
groove meningiomas which usually remain clinically
quiescent during the early phase of growth.
Anatomically, olfactory groove meningiomas arise from
the weakest part of the skull base, the cribriform
plate, which makes them prone to infiltrate the
underlying bone and extend into the paranasal sinuses
and nasal cavity. This is a rare feature in planum
sphenoidale or tuberculum sellae meningiomas.
A systematic assessment of functional outcome after
resection of olfactory groove meningiomas, particularly
in respect to olfactory function, has rarely been
performed [3, 30, 46]. We retrospectively analyzed
meningiomas with a predominant origin from the dura of
the cribriform plate with regard to clinical
presentation, different surgical approaches and
follow-up results which were treated microsurgically in
our institution.
Patients and methods
From June 1990 till June 2003, an olfactory groove
meningioma was microsurgically resected in 56
consecutive patients in our department. The medical
charts, surgical records and radiological studies were
retrospectively reviewed in these patients. Only tumours
with a primary origin from the dura of the cribriform
plate were included in this report. Lesions with a
predominant dural origin from the planum sphenoidale,
tuberculum sellae, anterior clinoidal process or orbital
roof were not considered in this series.
Radiological studies
Magnetic resonance imaging (MRI) was obtained
preoperatively in all patients and clearly demonstrated
the relationship of the tumour with the optic nerves,
chiasm and the anterior cerebral arteries (ACA). These
vessels were encased by the tumour in three patients. A
significant bifrontal or unilateral edema was displayed
on MRI in 34 patients. CT with bone algorithms,
performed preoperatively in 23 patients revealed a
hyperostosis of the crista galli or the cribriform plate
in six and erosion of the cribriform plate in four
cases. Cerebral angiography was performed regularly
early in the study period to demonstrate tumour
vascularity, provide information regarding ACA
displacement and to evaluate the possibility of
preoperative embolization. In all 23 cases studied
angiographically, the tumour was predominantly supplied
by the anterior or posterior ethmoidal branches of the
ophthalmic artery and preoperative partial embolization
was performed in two patients with occlusion of the
anterior branch of the middle meningeal artery.
Angiography is no longer performed in these tumours in
our institution. Mean maximal diameter of the tumours as
depicted from preoperative MRI was 5.2 cm (range:
2.57.5 cm).
Tumour extension and
dural attachment
As shown by preoperative MRI and confirmed
intraoperatively, the tumour was attached to the
cribriform plate, adjoining part of the planum
sphenoidale, crista galli and medial orbital roofs on
both sides in 24 patients. Tumours in these cases were
broad-based, were larger than 5.5 cm in maximal diameter
and had an almost symmetric growth on both sides. The
tumour attachment area was restricted to the cribriform
plate and adjacent part of the orbital roofs on both
sides in 19 patients.
A pure unilateral dural origin from the cribriform plate
and adjoining anterior cranial base was observed in 13
patients, on the left side in six and on the right side
in seven cases. Bilateral extension of the tumour into
the ethmoidal cells was disclosed on preoperative
coronal MRI in two cases and unilateral extension in
one. The tumour reached the nasal cavity in two
additional cases. The meningioma extended into the optic
canal on one or both sides in five patients, all of whom
had visual disturbances preoperatively.
Surgical approaches
Thirty-six patients with a bilateral tumour were
operated via a bifrontal craniotomy with opening of the
frontal sinus, double ligation and division of the
anterior end of the superior sagittal sinus with
subsequent subfrontal Fig. 3. Artists sketch showing
dural attachment of olfactory groove meningiomas. (A)
Bilateral attachment to the cribriform plate, planum
sphenoidale and orbital roofs (24 cases), (B) tumours
attached to the cribriform plate and medial orbital
roofs bilaterally (19 cases), (C) Unilateral attachment
to the cribriform plate and medial orbital roof (13
cases). Posterior extension over the tuberculum sellae
(straight arrow) was observed in four, encroachment into
the optic canal (curved arrow) in five cases removal of
the meningioma. This approach has been described in
detail [27, 28, 36]. Additionally, a bilateral tumour
was extirpated via a pterional approach in seven
patients. The contralateral tumour part was removed
after partial resection of the falx cerebri and crista
galli [15, 47]. Tumours restricted to one side were
resected through a unilateral frontal approach in four
cases, via a pterional approach in six and a lateral
supraorbital (key-hole) craniotomy in three patients
[35]. The latter approach was used in small tumours up
to 3.5 cm in diameter and was endoscopically-assisted in
one case with a deep olfactory groove. In all but three
patients were the tumour had been removed via a frontal
craniotomy the floor of the anterior cranial base was
covered with a vascularized galea-periosteal flap
reinforced with sutures and fibrin glue. A hyperostosis
of the crista galli and, or cribriform plate was removed
by drilling in 16 patients. Tumours that had invaded
into the ethmoidals or nasal cavity were removed via a
bifrontal craniotomy. This was combined with a lateral
rhinotomy performed by members of the otolaryngology
department in two cases.
Patients follow-up
All patients were followed-up with clinical examination
and MRI studies six months and one year after surgery.
Thereafter, patients were re-examined at one or two year
intervals based on each follow-up result. Postoperative
assessment of mental function was available in 25 of 31
patients with preoperative personality changes.
Olfactory function was tested semi-quantitatively before
surgery and on each follow-up examination with different
odours for each nostril separately. Preoperatively, test
results were reliably obtained in 46 patients. In the
remainder mental changes allowed only a gross
differentiation between smelling and not smelling at
best. Postoperative results of olfactory tests were
available for analysis in 41 patients. All patients with
visual disturbances had detailed pre- and postoperative
ophthalmological investigations, including visual
acuity, visual fields, fundoscopy and intraocular
pressure measurement.
Results
The 41 women and 15 men had a mean age of 51 years
(range 3074 years). The most common presenting symptoms
were mental disturbances in 22 patients (39.3%),
headache in 11 (19.6%), visual deterioration in nine
(16.1%) and anosmia in eight cases (14.3%).
References
1. Auque J, Civit T (1996) Superficial veins
of the brain. Neurochirurgie 42 Suppl 1: 88108
2. Bakay L (1984) Olfactory meningiomas. The missed
diagnosis. JAMA 25: 5355
3. Bakay L, Cares HL (1972) Olfactory meningiomas: report of
a series of twenty-five cases. Acta Neurochir (Wien) 26:
112
4. Bassiouni H, Hunold A, Asgari S, Stolke D (2004)
Meningiomas of the posterior petrous bone: functional
outcome after microsurgery. J Neurosurg 100: 10141024
5. Briant TDR, Zorn M, Tucker W, Wax MK (1993) The
craniofacial approach to anterior skull base tumors. J
Otolaryngol 22: 190194
6. Castillo M, Mukherji SK (1996) Magnetic resonance imaging
of the olfactory apparatus. Top Magn Reson Imaging 8: 8086
7. Chan RC, Thompson GB (1984) Morbidity, mortality, and
quality of life following surgery for intracranial
meningiomas. A retrospective study in 257 cases. J Neurosurg
60: 5260
8. Cushing H, Eisenhardt L (1938) The olfactory groove
meningiomas with primary anosmia. In: Cushing H, Eisenhardt
L (eds) Meningiomas. Charles C Thomas Springfield, pp
250282
9. Dandy WE (1925) Contributions to brain surgery: a removal
of certain deep-seated brain tumors. Ann Surg 82: 513520
10. DeMonte F (1996) Surgical treatment of anterior basal
meningiomas. J Neurooncol 29: 239248
11. Derome PJ, Guiot G (1978) Bone problems in meningiomas
invading the base of the skull. Clin Neurosurg 25: 435451
12. Durante F (1885) Estirpazione di un tumore endocranico.
Arch Soc Ital Chir 2: 252255
13. El Gindi S (2000) Olfactory groove meningioma: surgical
techniques and pitfalls. Surg Neurol 54: 415417
14. Guthrie BL, Ebersold MJ, Scheithauer BW (1990) Neoplasms
of the intracranial meninges. In: Youmans JR (ed)
Neurological Surgery vol 5. 3rd edn. WB Saunders,
Philadelphia, pp 32503315
15. Hassler W, Zentner J (1989) Pterional approach for
surgical treatment of olfactory groove meningiomas.
Neurosurgery 25: 942947
16. Karnofsky DA, Abelmann WH, Craver LF (1948) The use of
nitrogen mustards in the palliative treatment of cancer.
Cancer 1: 634656
17. Kempe LG (1968) Olfactory groove meningioma. In: Kempe
LG (ed) Operative neurosurgery, vol 1, 1st edn. Springer,
New York, pp 104108
18. Kennedy F (1911) Retrobulbar neuritis as an exact
diagnostic sign of certain tumors and abcesses in the
frontal lobes. Am J Med Sci 142: 355368
19. Keros P (1962) On the practical value of differences in
the level of the lamina cribrosa of the ethmoid. Z Laryngol
Rhinol Otol 41: 808813
20. Long DM (1989) Meningiomas of the olfactory groove and
anterior fossa. Atlas of operative neurosurgical technique,
cranial operations, vol 1. Lippincott Williams&Wilkins,
Baltimore, pp 238241
21. Maiuri F, Salzano FA, Motta S, Colella G, Sardo L (1998)
Olfactory groove meningioma with paranasal sinus and nasal
cavity extension: removal by combined subfrontal and nasal
approach. J Craniomaxillofac Surg 26: 314317
22. Mathiesen T, Linquist C, Kihlstreom L, Karlsson B (1996)
Recurrence of cranial meningiomas. Neurosurgery 39: 29
23. Mayfrank L, Gilsbach JM (1996) Interhemispheric approach
for microsurgical removal of olfactory groove meningiomas.
Br J Neurosurg 10: 541545
24. McDermott MW, Rootman J, Durity FA (1995) Subperiosteal,
subperiorbital dissection of the anterior and posterior
ethmoidal arteries for meningiomas of the cribriform plate
and planum sphenoidale: technical note. Neurosurgery 36:
12151219
25. Mirimanoff RO, Dororetz DE, Linggood RM, Ojemann RG,
Mortuza RL (1985) Meningioma: analysis of recurrence and
progression following neurosurgical resection. J Neurosurg
62: 1824
26. Obeid F, Al-Mefty O (2003) Recurrence of olfactory
groove meningiomas. Neurosurgery 53: 534543
27. Ojeman RG (1996) Supratentorial meningiomas: clinical
features and surgical management. In: Wilkins RH, Rengachary
SS (eds) Neurosurgery, vol 1. McGraw-Hill, New York, pp
873890
28. Ojemann RG (1991) Olfactory groove meningiomas. In:
Al-Mefty O (ed) Meningiomas. Raven Press, New York, pp
383393
29. Olivecrona H (1967) Surgical treatment of intracranial
tumors. In: Olivecrona H et al (eds) Handbuch der
Neurochirurgie, vol. 4. Springer, Berlin, pp 160167
30. Passagia JG, Chirossel JP, Favre JJ, Gray E, Reyt E,
Righini C, Chaffanjon P (1999) Surgical approaches to the
anterior fossa, and preservation of olfaction. Adv Tech
Stand Neurosurg 25: 195241
31. Persky MS, Som ML (1978) Olfactory groove meningioma
with paranasal sinus and nasal cavity extension: a combined
approach. Otolaryngology 86: 714720
32. Poppen JL (1964) Operative techniques for removal of
olfactory groove and suprasellar meningiomas. Clin Neurosurg
2: 17
33. Quest DO: Meningiomas (1978) An update. Neurosurgery 3:
219225
34. Ransohoff J, Nockels RP (1993) Olfactory groove and
planum meningiomas. In: Apuzzo MLJ (ed) Brain surgery.
Complication avoidance and management, vol. 1. Churchill
Livingstone, New York, pp 203219
35. Reisch R, Perneczky A, Filippi R (2003) Surgical
technique of the supraorbital key-hole craniotomy. Surg
Neurol 59: 223227
36. Samii M, Ammirati M (1992) Olfactory groove meningiomas.
In: Samii M (ed) Surgery of the skull base: meningiomas.
Springer, Berlin, pp 1525
37. Seeger W (1983) Microsurgery of the cranial base.
Springer, New York
38. Sekhar LN, Tzortzidis F (1999) Resection of tumors by
the frontoorbital approach. In: Sekhar LN et al (eds)
Cranial microsurgery: approaches and techniques. Thieme, New
York, pp 6175
39. Simpson D (1957) The recurrence of intracranial
meningiomas after surgical treatment. J Neurol Neurosurg
Psychiatry 20: 2239
40. Solero CL, Giombini S, Morello G (1983) Suprasellar and
olfactory meningiomas: report on a series of 153 personal
cases. Acta Neurochir (Wien) 67: 181194
41. Symon L (1977) Olfactory groove and suprasellar
meningiomas. In: Krayenbhuhl H et al (eds) Advances and
technical standards in Neurosurgery, vol 4. Springer, Wien
New York, pp 6791 120 H. Bassiouni et al.
42. Teonnis W (1938) Zur Operation der Meningeome der
Siebbeinplatte. Zentralbl Neurochir 1: 17
43. Tsikoudas A, Martin-Hirsch DP (1999) Olfactory groove
meningiomas. Clin Otolaryngol 24: 507509
44. Turazzi S, Cristofori L, Gambin R, Bricolo A (1999) The
pterional approach for the microsurgical removal of
olfactory groove meningiomas. Neurosurgery 45: 821826
45. Van Toller S (1999) Assessing the impact of anosmia:
review of a questionnaires findings. Chem Senses 24:
705712
46. Welge-Luessen A, Temmel A, Quint C, Moll B,Wolf S,
Hummel T (2001) Olfactory function in patients with
olfactory groove meningioma. J Neurol Neurosurg Psychiatry
70: 218221
47. Yasargil MG (1996) Microneurosurgery of CNS Tumors, vol
IVB. Thieme, New York, pp 140141
|
Comments
 |
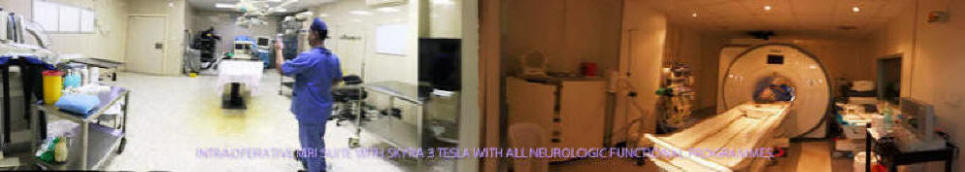
Intraoperative navigation will ameliorate such
events, and confirm the necessity for such technology. Real-time
intraoperative navigation is costly and commercially inapplicable
for private sector, and must be modified to be used for all surgical
disciplines and to have neurophysiologic monitoring added to the
navigation system merged with the visual data in real time.
|
 |
MRI of the brain done 01-January-2005 confirming the total
resection of the tumor with mild malacia of the left frontal lobe
due to to pressure effect of the missed right occipito-parietal
extradural hematoma. |




Postoperative MRI after 3 years showing complete resection and no
recurrence.
Olfactory groove meningiomas:
functional outcome
in a series treated microsurgically
H. Bassiouni, S. Asgari,
and
D. Stolke
Department of Neurosurgery, University Hospital Essen,
Essen, Germany
 |
Background
A systematic investigation of long-term follow-up
results after microsurgical treatment of patients harbouring
an olfactory groove meningioma, particularly with regard to
postoperative olfactory and mental function, has rarely been
performed. We reassessed a series of patients treated
microsurgically for an olfactory groove meningioma in regard
to clinical presentation, surgical approaches and long-term
functional outcome. Method. Clinical, radiological and
surgical data in a consecutive series of 56 patients
suffering from olfactory groove meningioma were
retrospectively reviewed.
Findings. Presenting symptoms of the 41 women and 15 men
(mean age 51 years) were mental changes in 39.3%, visual
impairment in 16.1% and anosmia in 14.3% of the patients.
Preoperative neurological examination revealed deficits in
olfaction in 71.7%, mental disturbances in 55.4% and reduced
vision in 21.4% of the cases. The tumour was resected via a
bifrontal craniotomy in 36, a pterional route in 13, a
unilateral frontal approach in 4 and via a supraorbital
approach in 3 patients. Extent of tumour resection according
to Simpsons classification system was grade I in 42.9% and
grade II in 57.1% of the cases. After a mean followup period
of 5.6 years (range 113 years) by clinical examination and
magnetic resonance imaging (MRI), 86.8% of the patients
resumed normal life activity. Olfaction was preserved in
24.4% of patients in whom pre- and postoperative data were
available. Mental and visual disturbances improved in 88 and
83.3% of cases, respectively. Five recurrences (8.9%) were
observed and had to be reoperated.
|
 |
Conclusions
Frontal approaches allowed better resection of
tumours with gross infiltration of the anterior cranial
base, tumours extending into the ethmoids or nasal cavity
and in cases with deep olfactory grooves. Preservation of
olfaction should be attempted in patients with normal or
reduced smelling preoperatively. |
 |
Introduction
Meningiomas of the midline anterior skull base
include tumours originating from the dura of the cribriform
plate, planum sphenoidale and tuberculum sellae and account
for about 10% of all intracranial meningiomas [41]. For
clinical, radiological and surgical purposes true olfactory
groove meningiomas, i.e. tumours originating from the dura
between the crista galli and the frontosphenoid suture
should be differentiated from planum sphenoidale and
tuberculum sellae meningiomas [8, 32]. Tumours arising from
the latter sites usually come to clinical attention at an
early stage with visual deterioration, while this is a late
feature in olfactory groove meningiomas which usually remain
clinically quiescent during the early phase of growth.
Anatomically, olfactory groove meningiomas arise from the
weakest part of the skull base, the cribriform plate, which
makes them prone to infiltrate the underlying bone and
extend into the paranasal sinuses and nasal cavity. This is
a rare feature in planum sphenoidale or tuberculum sellae
meningiomas.
A systematic assessment of functional outcome after
resection of olfactory groove meningiomas, particularly in
respect to olfactory function, has rarely been performed [3,
30, 46]. We retrospectively analysed meningiomas with a
predominant origin from the dura of the cribriform plate
with regard to clinical presentation, different surgical
approaches and follow-up results which were treated
microsurgically in our institution. |
 |
Patients and methods
From June 1990 till June 2003, an olfactory
groove meningioma was microsurgically resected in 56
consecutive patients in our department. The medical charts,
surgical records and radiological studies were
retrospectively reviewed in these patients. Only tumours
with a primary origin from the dura of the cribriform plate
were included in this report. Lesions with a predominant
dural origin from the planum sphenoidale, tuberculum sellae,
anterior clinoidal process or orbital roof were not
considered in this series. |
|