
AVOIDANCE OF COSMETIC DEFORMITY DURING TRANSPETROSAL PRESIGMOID
APPROACH TO PETRO-CLIVAL REGION
M.A.Elias M.D., Ph.D.
Al-Bashir Hospital . MOH
Amman-Jordan
Published: 12-January-1996
OBJECTIVES: New approach to petroclival lesions through transpetrosal-presigmoid osteoplastic craniotomy without causing postoperative cosmetic deformities.
TECHNIQUES: During the last 4 years, 20 operations were performed ( 10 giant acoustic neuromas, 4 meningiomas, 1 ependymoma , 2 teratomas, 1 clival chordoma , 1 retrosellar craniopharyngioma and 1 glomus jugulare tumor with chronic persistent otitis media), using this technique. High speed drill, loupes and preoperative temporal bone window CT-scan are prerequisites. The raised bone flap include part of the retrosigmoid, the mastoid outer shell with the mastoid tip. The posterior wall of the bony external meatus is left intact. Insertion of small 3 mm holes behind the external meatus and beneath the skeletonized mastoid tip parallel to the insertion of the digastric muscle, and drilling over the sigmoid sinus from behind and antesigmoidally to meet the drilling performed in the superior surface of the retrolabirinthine part of the temporal bone, 10 mm anterior to the petro-sigmoid junction. The deeper procedures such as translabirinthine, transcochlear, facial nerve transposition, are done as described elsewhere. The mastoid cavity within the bone flap is drilled to prevent musicale formation. The free spaces formed after setting back the flap is filled by autologeous muscle graft.
RESULTS: No cosmetic deformity was noted after these procedures. The technique can be applied even in the presence of chronic infection. No complication, associated with this technique was recognized during 50 months.
CONCLUSION: A technique, which needs more effort from the surgeon to perform, eliminates the cosmetic disfigurement after approaching the petroclival region .
Key words : Petroclival tumor , Reconstruction, Surgical approach, Transpetrosal-transtentorial approach.
During the last ten years , the posterior transpetrosal -transtentorial approach regained popularity to reach the petroclival region and difficult lesions of the pontocerebellar region. The pioneering work and experience of the otolaryngeal skull base surgeons for more than forty years, were the fundament upon which , the posterior transpetrosal approaches came to a reality (4). The work of Al-Mefty O. et al and Sami M. et al inaugurated the theoretical background for the posterior transpetrosal -transtentorial approaches (1,8,11,12,13,21 and 22) . However, the cosmetic disfigurement in the retroauricular region after the posterior transpetrosal-transtentorial approaches is unsatisfactory. In the last 5 years several reports appeared in the literature handling this problem . We have devised a new technique in performing the osteoplastic craniotomy during the posterior transpetrosal-transtentorial approaches to avoid the cosmetic disfigurement.
OPERATIVE TECHNIQUES
Most of our patients were operated in the supine or park bench position when posterior transpetrosal-transtentorial approach was contemplated. Avoidance of the sitting position was due to frequent traction injury to the basal parts of the exposed temporal lobe triggered by gravity . The posterior limb of the skin incision was extended a little far 3 cm below the level of the mastoid tip . During reflection of the cutaneo-subcutaneous flap, special attention to preserve the periosteum covering the mastoid plane behind the spine of Henli was paid. The temporalis muscle is dissected at its posterior attachment sharply and using the cutting diathermy dissected and reflected anteriorly. Most of the periosteum covering the mastoid plane is dissected and reflected anteriorly to the side of the external meatus, which is maximally skeletonized at the boundaries of the posterior wall of the bony external ear. Using cutting diathermy the sternocliedomastoid muscle and other running muscles lying beneath it are detached to expose the mastoid tip down to the digastric groove and the lateral half of the bone overlying the ipslateral cerebellar convexity. It is mandatory to stick properly to the bony boundaries and not to reach the stylomastoid foramen exit. In the nearby of the digastric groove most of the time there was an arterial bleeding , which was easily controlled. Bone wax was avoided in bleeding from the retromastoid emissaries and surgicele was used instead. If it failed then controlled amount of wax was used trying not to insert the wax blindly.
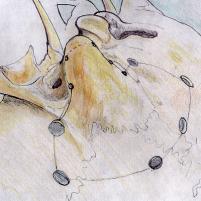
The osteoplastic bony flap was performed in the following manner ( Figure. 1) : That part overlying the convexital surface of the temporal and cerebellar hemishere was performed in the usual manner, taking into consideration that part crossing the transverse sinus. It is necessary to mention that , the next steps of the operation were performed with use of binocular loupes with 4.5 magnification with a high speed drill. Two important burr holes play the integral part of performing the remaining part of the flap . The first is located at the Henli spine abutting the superior wall of the bony external meatus. Usually a burr hole 7-8 mm diameter is sufficient to perform drilling down and behind toward the petrous ridge, trying to be all the time parallel to the external shell of the mastoid . Usually the plane of drilling will be 60 degrees to the axis of the petrous ridge and it will be at least 10 mm behind the arcuate eminence. The depth of dissection at that level will be 18± 4 mm and the gap created about 6-9 mm .The dura is used for guidance at this stage. At the depth of the drilling 10 mm space is created in downward direction at the Trautmann triangle , leaving a thin layer of bone , which is actually the bone overlying the sigmoid sinus. To regain adequate vision drilling is directed to the outer surface of the mastoid shell. For this stage we usually used the straight cutting rounded 3 mm diameter burr. Using the same burr or a 5 mm diameter one another burr hole is done at the continuity of the digastric groove behind the mastoid . The burr hole is extended anteriorly with a gap of 7-8 mm which will be actually transgresses the mid of the sigmoid sinus . A thin layer of bone is left and drilling is also directed parallel to the plane of the mastoid shell . This drilling is done until it unite with the superiorly done drilling . The sigmoid sinus all the time was transgressed during this second stage and the wide drilling space can be done , exposing during that the sigmoid sinus for more than 15 mm without causing any violation to the outer prominent contour of the mastoid shell. About 4-5 small burr holes are made at the circumference of the mastoid , so that the line is transecting the mastoid tip . The drilling is done in each hole so that it unite with the neighboring one just below the shell surface . These burr holes are united by oscillating small saw , minichisel or microosteotome. Usually there will be a feeling that the flap is moving at this stage. In the case that the flap is still not moving check for the left bony layer which covers the sigmoid sinus is needed and further thinning of this layer sometimes is needed. It is mandatory to elevate the flap gradually checking for the draining emmissaries , which could be coagulated and bisected.
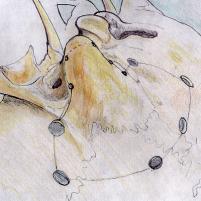

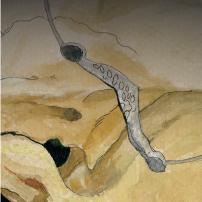
Figure. 1 : Schematic drawing demonstrating the burr holes , their diameter and the exposed field after flap elevation and projection of the drilling from inside.
It is mandatory to perform the drilling all the time near the outer surface of the mastoid shell. Despite that, some air cells left in the lower part of the flap are needed to be drilled out to prevent subsequent infection and mucocele formation. It is mandatory when to perform such a procedure to have preoperative CT-scan of the temporal bone with bone window to identify the relationship of the facial nerve, the degree of mastoid pneumatization, the localization of the PSC and the arcuate eminence. There was no single case where the procedure was impossible to perform, but it was different in the level of difficulty. With experience it became more familiar and easier to perform and it took around 30 min. to perform of the operating time. The compact type of mastoid with sclerotic bone was an added difficulty factor to the operative procedure.
The next steps of the operative protocol either retrolabirinthine, translabirinthine or transcochlear were performed as described by many authors ( 1,3,4 ,6,8,11,12,13,16,17,21,22,24,25,30 and 31 ).
After dural closure we all the time harvested a muscle from the quadriceps femoris to fill the space created . The bony flap was returned to its place and we feel that the mastoid cavity at the created flap hold the muscle graft as a spoon. The bone edges are usually smooth at the outer contours , and there could be gaps behind and underneath the mastoid shell over the trajectory of the sigmoid sinus. The burr hole defect performed at the spine of Henli is filled by bone dust obtained at the start of the operation. The following closure procedures are routine. Special attention must be paid to approximate and stitch the sternocliedomastoid muscle attachment with anteriorly and posteriorly reflected periosteal flaps over the mastoid.
During the last 50 months in the period 1993-1997 all the patients undergoing such an approach , avoidance of cosmetic deformity was achieved. Pathological picture of the patients is listed in table 1.
Table - 1
CHARACTER OF PATIENTS UNDERGOING OSTEOPLASTIC CRANIOTOMY WITH AVOIDANCE OF COSMETIC DISFIGUREMENT DURING POSTERIOR TRANSPETROSAL TRANSTENTORIAL APPROACH
|
PATHOLOGY |
NUMBER OF CASES |
|
|
|
|
Giant acoustic neurinomas |
10 |
|
Clival and petroclival meningiomas |
4 |
|
Giant petroclival teratoma |
2 |
|
Pontocerebellar angle ependymoma |
1 |
|
Retrosellar craniopharyngioma |
1 |
|
Glomus jugulare tumor |
1 |
|
Clival chordoma |
1 |
|
Total |
20 |
It is worthy to denote that half of the patients were operated elsewhere by other routes and came to us for reoperation . This fact played a little role since the previously attempted approaches were out of the mastoid area. At the same time, it played a major role inside, where the failed attempted dissection was done. It can be stated without hesitation that, there was no single complication related to the described modification. In one case during the elevation of the flap , one emmissary vein could not be controlled by coagulation and it was necessary to stitch the sigmoid sinus after flap reflection . In several occasions we attempted to perform drilling around the exit of the emmissary vein to isolate the venous wall and dissect and coagulate it. This step is felt to lessen the possibility of such complication. In another similar situation a dural sinus was running from above , over the temporal convexity down to the superior petrosal sinus 3 cm anterior to the sino-sigmoid junction.. Tear of the running dural vein took place and it was possible to control it by packing the dural venous structure by surgicele.


Figure.2 : Postoperative condition of scar without any bony deformity in the retroauricular region . The scar is seen running far behind and below the level of the mastoid tip.
The glomus jugulare patient had infected tumor with a gush of pus coming out the ear. She was operated elsewhere , and biopsy through the ruptured drum was performed .After several weeks of antibiotic treatment, operation was performed and antibiotic covering was held for three months after the operation. When the treatment was stopped the pus reappeared , with fistula from the drum. Conservative treatment for over the next six months could resolve the problem. The bone construct and the filling muscle kept their acceptable state all the time.
The retroauricular space was almost normal in shape in all patients after the operation . A slight thinning of the cutaneous layer with occasional discoloration was noted
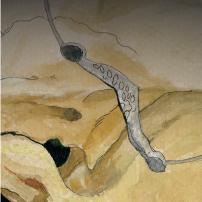
CT-scan of the temporal bone -bone window was performed to evaluate the condition of the construct. In some patients 3-D reconstruction was done ( Figure. 3,4 and 5 ).
Figure 3. : Immediate postoperative CT-scan demonstrating the flap position and the residual clot at the tumor bed site after removal of the clival chordoma through left-sided posterior transpetrosal retrolabirinthine approach.
     |
 |
Figure 3. 3-D reconstruction of the cranial base after left sided posterior transpetrosal approach from different angles, demonstrating the intact outer contours of the mastoid area at the site of attack. The other side presented for comparison. Note that the patient has also residual of the failed attempted attack to the lesion through anterior subtemporal area performed elsewhere prior to admission to our department.

Figure. 4 : Temporal bone window CT-scan demonstrating the condition of the left mastoid after posterior transpetrosal retrolabirinthine approach. Note , despite the anatomical continuity there is slight resorption of the cortical bone of the mastoid 5 months after the operation. Note also the pneumatization which appeared , suggesting either incomplete drilling of the pneumatized parts of the bone flap or the reappearance of the pneumatization later.
The posterior transpetrosal-transtentorial approaches require removal of varying amounts of the mastoid and petrosal bone, resulting in large retroauricular bone defect. In the last 5 years several authors started to publish options for resolving or avoiding such deformity ( Table. 2 ). Most of them have their positive and negative effects on the patient. The option proposed by Ramina R et al cannot be considered as a solution for the cosmetic disfigurement, since the bony contour is lost. The options proposed by Couldwell W , and Fukushima detach the mastoid shell of the remnant of the bony flap , making it more susceptible to infection and resorption or simply detachment. Using Gigli saw to harvest the en block petrosectomy as proposed by Sasaki T et al can cause damage to important vital structures. Filling the bone defect by hydroxyapatite cement is not always feasible, especially near a potentially dirty area such as the middle ear. Incomplete destruction of the bone chips with the accompanying mucosa, which were used by Tokoro K. et. al. to fill the bone defect hide a real danger for mucocele formation and infection. The suggestions proposed by Sekhar L and Nakamura M. et al. using the split bone graft still has a poor fixation quality in the case of the appearance of infection . The titanium mesh used by Zimmerman M et al. despite its inert character , remain a foreign body susceptible to infection.
Table - 2
PROPOSED OPTIONS TO RESOLVE THE COSMETIC DISFIGUREMENT OF RETROAURICULAR AREA AFTER POSTERIOR TRANSPETROSAL TRANSTENTORIAL APPROACHES
AUTHOR | DATE OF PUBLICATION |
REMARKS |
| |
|
Ramina R. et al. 20. | 1993 |
Z-plasty of the temporalis muscle with suturing to the sternocliedomastoid muscle without bone reconstruction |
Couldwell W.T and Fukushima T.2. | 1993 |
Cosmetic mastoidectomy using oscillating saw with high speed drill with subsequent fixation of the mastoid shell by miniplates |
Sasaki T. et al 23. | 1995 |
En block petrosectomy using Gigli saw |
Kveton J. F. et al. 14. | 1995 |
Filling the defect with hydroxyapatite cement |
Tokoro K. et al 32. | 1996 |
Filling the defect by bone chips mixed with fibrin glue |
Sekhar L. N. and Morita A. 29. | 1996 |
Fitted calvarial piece fixed by titanium miniplates |
Nakamura M. et al. 18 | 1997 |
Reconstruction using a split bone graft fixed by nylon |
Zimmerman M., Seifert V. 33. | 1997 |
Reconstruction using titanium mesh fixed with titanium miniplates |
Elias M.A. | Recent demonstration |
Osteoplastic craniotomy during which the outer shell of the mastoid is included with the bony flap, using the high speed drill |
Despite the fact, that our option took place in practice prior to the emergence of most of the proposed options , it has it’s advantage that the bone flap is the most stable one in these options and the most resistant in the case of the de novo appearance or continuity of previous infection. It is realized that this option is time consuming , and the possibility of draining veins laceration during flap elevation still remain.
To overcome these negative effects the introduction of proper dissecting tools and the learning curve can minimize the negative effects of the proposed option.
References :
1. AI-Mefty 0, Fox JL, Smith RR: Petrosal approach for petroclival meningiomas. Neurosurgery 22:510-517, 1988.
2. Couldwell WT, Fukushima T: Cosmetic mastoidectomy for the combined supra/infratentorial transtemporal approach: Technical note. J Neurosurg 79:460-461, 1993.
3. Fisch U& Douglas Mattox. Microsurgery of the Skull Base. 1988. George Thieme Verlage Stuttgart. New York.
4. Frodel JL, Marentette JL, Quatela VC, Weinstein GS: Calvarial bone graft harvest: Techniques, considerations, and morbidity. Arch Otolaryngol Head Neck Surg 119:17-23, 1993.
5. Fukushima T: Combined supra- and infra-parapetrosal approach for petroclival lesions, in Sekhar LN, Janecka IP(eds): Surgery of Skull Base Tumours. New York, Raven Press, 1993, pp 661-670.
6. Gardner G. et al. Transtemporal approaches to the posterior cranial fossa . Operative Neurosurgical Techniques Henry H.Schmidek and William H.Sweet. Third Edition. 1995. W.B.Saunders Company. 843-850.
7. Gormley WB, Fukushima T, Chen D: En bloc petrosectomy for petroclival lesions. J Neurosurg 84:536, 1996 (letter).
8. Haddad GF, AI-Mefty 0: Lateral "presigmoid" approach to the clivus, in Torrens M, AI-Mefty 0, Kobayashi S (eds): Operative Skull Base Surgery. Edinburgh, Churchill Livingston, 1997, pp 313-320.
9. Hakuba A, Nishimura S: Total removal of clivus meningiomas and the operative results. Neurol Med Chir (Tokyo) 21:59-73,1981.
10. Hakuba A, Nishimura S, Jang Bj: A combined retroauricular and preauricular transpetrosal-transtentorial approach to clivus meningiomas. Surg Neurol 30:108116, 1988.
11. Hitselberger WE, House WF: A combined approach to the cerebellopontine angle: A suboccipito-petrosal approach. Arch Otolaryngol 84:267-285, 1966.
12. John T. McElveen, Jr. The translabirinthine approach to cerebellopontine angle tumours. Neurosurgery. Robert H.Wilkins , Setti S. Rengachary Second Edition. 1996. McGraw-Hill. 1107-1113.
13. King T.T. , O'Connor: Translabirinthine approach to acoustic neuromas. Operative Neurosurgical Techniques Henry H.Schmidek and William H.Sweet. Third Edition. 1995. W.B.Saunders Company. 813-827.
14. Kveton JF, Friedman CD, Constantino PD: Indications for hydroxyapatite cement reconstruction in lateral skull base surgery. Am J OtoI 16:465-469, 1995.
15. MacCarthy JG, Zide BM: The spectrum of calvarial bone grafting: Introduction of the vascularized calvarial bone flap. Plast Reconstr Surg 74:10-18,1984.
16. Miller CC, van Loveren HR, Keller JT, Peusak M, El-Kalliny M, Tew JM: Transpetrosal approach: Surgical anatomy and technique. Neurosurgery 33:461-469, 1993.
17. Morrison AW, King TT: Experiences with a translabirinthine-transtentorial approach to the cerebello-pontine angle: Technical note. J Neurosurg 38:382-390, 1973.
18. Nakamura M., Tamaki N., Hara Y., Nagashima T., Tamura S. :Use of split bone graft to correct the cosmetic deformity associated with the transpetrosal-transtentorial surgical approach: Technical report. Neurosurgery, Vol. 40, 1089-1091, 1997
19. Ojemann R.G. Suboccipital transmeatal approach to vestibular schwannoma . Operative Neurosurgical Techniques Henry H.Schmidek and Wiliam H.Sweet. Third Edition. 1995. W.B.Saunders Company. 829-841. S. Rengachary Second Edition. 1996.
20. Ramina R, Maniglia J, Barrionuevo CE: Surgical excision of petrous apex lesions, in Sekhar LN, Janecka IP (eds): Surgery of Cranial Base Tumours. New York, Raven Press, 1993, pp 291-305.
21. Samii M, Ammirati M: The combined supra-infratentorial pre-sigmoid sinus avenue to the petro-clival region: Surgical technique and clinical applications. Acta Neurochir (Wien) 95:6-12, 1988.
22. Samii M, Ammirati M, Mahran A, Bini W, Sepehrnia A: Surgery of petroclival meningiomas: Report of 24 cases. Neurosurgery 24:1217,1989.
23. Sasaki T, Taniguchi M, Suzuki 1, Kirino T: En bloc petrosectomy using a Gigli saw for petroclival lesions. J Neurosurg 83:559-560,1995.
24. Sato 0 : Transoccipital transtentorial approach for removal of cerebellar haemangioblastoma. Acta Neurochir (Wien) 59:195, 1981
25. Schmidek H.H. Surgical management of cerebellar tumours in adults . Operative Neurosurgical Techniques Henry H.Schmidek and William H.Sweet. Third Edition. 1995. W.B.Saunders Company. 791-800.
26. Seifert V, Stolke D: Posterior transpetrosal approach to basilar trunk and vertebrobasilar junction aneurysms. J Neurosurg 85:373-376,1996.
27. Sekhar LM, Estonillo R: Transtemporal approach to the skull base: An anatomical study. Neurosurgery 19:799-808, 1986.
28. Sekhar LN, Swamy NKS, jaiswal V, Rubinstein E, Hirsch WE Jr, Wright DC: Surgical excision of meningiomas involving the clivus: Preoperative and intraoperative features as predictors of postoperative functional deterioration. J Neurosurg 81:860-868, 1994.
29. Sekhar LN, Morita A: Cosmetic reconstruction after mastoidectomy for the transpetrosal-presigmoid approach: Technical note. Neurosurgery 39:188, 1996 (comment).
30. Spetzler R.F, Daspit CP, Pappas CTE: The combined supra- and infratentorial approach for lesions of the petrous and clival regions: Experience with 46 cases. J Neurosurg 76:588-599, 1992.
31. Tarlov E.C. Surgical management of tumours of the tentorium and clivus. Operative Neurosurgical Techniques Henry H.Schmidek and William H.Sweet. Third Edition. 1995. W.B.Saunders Company. 783-788.
32. Tokoro K, Chiba Y, Murai M, Hayashi A, Kyurna Y, Fuju S, Yamamoto 1: Cosmetic reconstruction after mastoidectomy for transpetrosal-presigmoid approach: Technical note. Neurosurgery 39:186-188, 1996.
33. Zimmerman M., Seifert V. : Anatomic reconstruction of the posterolateral cranial base with titanium micromesh for combined transpetrosal approach : Technical Note. Neurosurgery 41: 983-986, 1997
The author have made every effort to trace the copyright holders for borrowed material. If inadvertently overlooked any, will be pleased to make the necessary arrangements at the first opportunity.