|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Most of the site will reflect the ongoing surgical activity of Prof. Munir Elias MD., PhD. with brief slides and weekly activity. Functional Neurosurgery Neuroradiological Sites NeuroSience Sites
Inomed Stockert Neuro N50. A versatile
Multigen RF lesion generator . |
 |
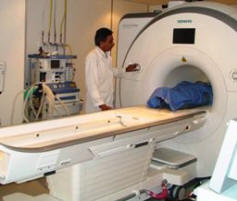 Skyra MRI with all clinical applications in the run since 28-Novemeber-2013.
Leica HM500
After long years TRUMPF TruSystem 7500 is running with in the neurosuite at Shmaisani hospital starting from 23-March-2014
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
ELECTROCOAGULATION IN TRIGEMINAL NEURALGIA Over most of century, a variety of neurosurgical operations and procedures have been introduced to treat trigeminal neuralgia, each with its enthusiasts and each with its period of vogue or place of popularity. The objective of almost all these treatments has been the creation of a sensory deficit in the area of pain, especially in the trigger area. Major intracranial operative procedures, with their attendant risks, gave way in many places to percutaneous approaches to the ganglion and retrogasserian rootlets for the instillation of alcohol, boiling water, phenol, glycerol, etc. In the early 1930s, Kirschner introduced his technique of electrocoagulation of the gasserian ganglion using a diathermy apparatus. He developed an innovative stereotactic device to aid in penetrating the foramen ovale, which was widely used in European centers. A problem with this technique was lack of control over the extent and location of the sensory deficit. Recognizing the deficiencies in the Kirschner technique. Sweet in 1970 introduced the radiofrequency (RF) technique. which significantly improved the control of the lesion. White and Sweet in 1955 declared. "As with alcohol injection, avoidance of denervation of the cornea seems the major unsolved problem. If we can: (1) consistently destroy the 2nd and 3rd divisions while saving the first and other nearby structures; (2) lower the rate of recurrence: and (3) keep the mortality near zero, many more surgeons will take it up. As far as we know no one has quite demonstrated this degree of skill." It is readily admitted. however, that an entirely satisfactory surgical method of treating trigeminal neuralgia is still not available. That ideal treatment would have to be safe, to leave the patient with no sensory deficit in the face, and to have no significant incidence of recurrence of pain. Indications and Preoperative Evaluation Carbamazepine, either alone or in combination with baclofen or phenytoin, has unquestionably proved to be the mainstay of the medical treatment of this disease. The primary indication for electrocoagulation then is refractoriness to this drug or inability to tolerate its side effects, the most common of which are ataxia, drowsiness, gastrointestinal distress, mental confusion, and rash. Patients who are elderly or who either are not a good risk for a major intracranial procedure or fear such a procedure would also be candidates. Patients who have had a peripheral block and liked the result despite facial numbness may opt for radiofrequency treatment. Finally, some patients find a more benign, less time-consuming, and less expensive form of treatment more attractive than a major intracranial operation. This procedure is good only for patients with true trigeminal neuralgia. the diagnosis of which is easily made from a careful history. The atypical facial neuralgias may only be made worse. Informed consent concerning the permanency of sensory deficits. the possibility that pain may recur and require another treatment, the possibility of corneal anesthesia and its consequences, and the possibility of annoying sensations in the face is obtained the day before the procedure. Prior to the treatment an enhanced CT or MRI scan should be performed to rule out the remote possibility of a cerebellopontine angle tumor or a vascular lesion. A hematologic profile is recommended by some to ensure there is no underlying bleeding diathesis related to ongoing medication. Advantages and Disadvantages The procedure is easily performed with minimal risk to the patient. It can readily be repeated if necessary. It is well tolerated by the elderly and avoids a major operative procedure in the poor-risk patient. Facial paralysis does not occur. When facilities permit, it can be performed on an outpatient basis. A potential problem with this procedure is that the face can very easily be made too numb. leading to the development of annoying paresthesia and dysesthesia in the areas of sensory deprivation. This outcome may result either from a misguided surgeon who goes for a sure cure and creates unnecessarily dense numbness or from the use of a technique that does not permit careful ongoing monitoring of the location and extent of the sensory deficit as it is being created. It is remarkable how little sensory deficit is necessary to provide lasting relief in many patients. The most extreme version of the annoying sensations that may accompany excessive numbness is anesthesia dolorosa. a condition in which there is a constant scratching, burning. or itching sensation in the face, eye, or mouth that is impossible to relieve. Approximately 6 percent of patients have paresthesia and dysesthesia resulting from treatment which they consider to be annoying, although the incidence of true anesthesia dolorosa should be 1 percent or less. Another problem. if careful technique is not used, is loss of the corneal reflex. with the risk of neurolytic keratitis and the potential for blindness. A late recurrence rate of approximately 27 percent is acceptable, since it is simple to repeat the procedure. Most patients request retreatment at the first mild recurrence of pain. and some opt for or even demand, immediate retreatment rather than resuming medication. Technique Two methods for performing the RF thermocoagulation procedure are described here: one using a temperature-monitoring electrode and another, using a small cordotomy-type electrode. Other variations in the procedure that are described are the anesthetic technique and the methods used in penetrating the foramen ovale. The Electrode The primary advantage of the smaller cordotomy-type electrode is that the lesion can be made with the patient awake so that constant monitoring can be employed. This possibility relates to the fact that thermocoagulation of the gasserian ganglion and the divisions distal to the ganglion causes intolerable pain. whereas coagulation of the retrogasserian rootlets causes very little. or at least tolerable discomfort. Monitoring of the patient during lesioning ensures that corneal sensation is being maintained. that sensory deficits are not being created in unwanted areas. and that too much sensory deficit is not being inflicted. Temperature monitoring is not available with this electrode, but patient monitoring is far more effective than temperature monitoring. Furthermore. the temperature required to make a lesion varies according to the proximity of the electrode to the retrogasserian rootlets. Lower temperatures are required if the electrode is within the rootlets. and higher temperatures if it is merely in their vicinity. In one series. using the temperature monitoring electrode, the final temperatures ranged from 47° to 108°. This variability emphasizes the unreliability of depending on temperature alone. The electrode has a bared tip 0.4 mm in diameter and 3 mm long. Its insulation protrudes 2 mm beyond the tip of a thin-walled 18-gauge lumbar puncture (LP) needle (3 mm bare and 2 mm insulated). The exposed tip is bent to permit lateral deviation of the tip when the electrode assembly is rotated within the LP needle. The hub of the LP needle acts as the indifferent or ground electrode. and the bare electrode tip acts as the active electrode. This smaller electrode makes it possible to spare the third division in cases of isolated second-division trigeminal neuralgia, in the majority of cases. Patients appreciate this, in that they do not like a numb third division when they have no pain there. A disadvantage of the cordotomy-type electrode is that precise localization of the electrode within the rootlets is not always easy to achieve; skill in the use of the needle must be developed. Also. because this electrode is smaller. it has a higher current density and a greater tendency to cause boiling. If boiling occurs, a gas bubble forms, the milliamperage falls off, the voltage rises and current flow ceases. A larger lesion cannot be made at that location, and the electrode must be moved to a new location if the procedure has not been completed. Nevertheless, Tew, Sweet and others think that temperature monitoring is an important adjunct. The temperature-monitoring electrode they use requires a second indifferent or ground electrode, which may be a cautery plate or a needle In the forehead or arm. A burn can occur at the site of the indifferent electrode. The patient must be protected against pain during the creation of the RF lesion with the short-acting anesthetic methohexital. The curved temperature-monitoring electrode developed by Tew offers considerable advantage over the straight 7.5-mm temperaturemonitoring electrode that was widely used in the past. A temperaturemonitoring electrode with an active surface of 5 mm or less is recommended. A small cordotomy-type electrode, similar to the one described above, with temperature monitoring capabilities is now available. Anesthetic Technique No premedication is used, but on the patient's arrival in the treatment room, 2 mg of diazepam or 1 mg of medazolam is given intravenously along with 0.05 to 0.1 mg of fentanyl. Additional fentanyl may be required. It must be remembered that too much of this medication may make it difficult for elderly patients to fully cooperate when the extent of the sensory deficit is evaluated. The needle site in the cheek is infiltrated with 1% lidocaine. This provides local anesthesia and distends the cheek to help prevent penetration of the oral cavity. If a long needle is used here, there is some risk of anesthetizing the third division as it emerges from the foramen ovale, which would preclude satisfactory treatment of the third division. The only time we put the patient to sleep is when the needle is passed through the foramen ovale, which is often the most painful part of the procedure. The short-acting agent methohexital is then used. Between 30 and 50 mg is usually adequate. Patients who underwent the procedure using only diazepam and fentanyl and then returned and had a second procedure with methohexital were universally most grateful for the change. At the time of penetration of the foramen ovale, or during the lesioning, there may be a remarkable hypertensive burst in some patients, and deaths have been reported from hypertensive intracerebral hematomas. The anesthesiologist should therefore be warned of this possibility, an arterial line inserted, and measures to control hypertension made available for immediate use. Continuous monitoring of the ECG is also advised. If the larger temperature-monitoring electrode is used, it is usually necessary to use methohexital each time a lesion is made, although in some cases it is possible to keep the patient awake after the initial lesions have been made. With the proper anesthetic technique, which apparently provides some amnesia for the event, and a lesion made in the retrogasserian rootlets rather than the ganglion, this should not be a particularly painful procedure. That this is true is evidenced by the readiness with which patients return for retreatment when it is necessary. With some experience, one should be able to perform the treatment in 45 min or less. Penetration of the Foramen Ovale It is most important to appreciate that ordinarily the least difficult aspect of the technique is the penetration of the foramen ovale. Several techniques have been recommended. Härtel Technique Most techniques use the Härtel landmarks initially. The needle insertion site is 2.5 to 3.0 cm lateral to the corner of the mouth more medial for third-division lesions and more lateral for firstdivision lesions. Often the needle insertion site is a little inferior to a point directly lateral to the corner of the mouth. A finger must be placed in the patient's mouth to avoid penetrating the oral mucosa. Meningitis is a recognized complication of this procedure. In the frontal view the needle is directed toward the pupil, and on the lateral view it is directed toward a point on the zygoma 2.5 cm anterior to the anterior aspect of the ear canal. It may be possible to pass the needle through the foramen ovale using only these landmarks, but that is not recommended, because without additional radiographic assistance the carotid artery may be punctured or the needle may enter the superior orbital fissure. The optic nerve has been penetrated by this technique. Lateral and Anteroposterior Radiographic Landmarks It is recommended that an image intensifier be used at this point to visualize the lateral orientation of the needle, which should be aiming at the vertex of the angle produced by the shadows of the clivus and the petrous ridge. It is better to enter on the high side of this point, because a lower orientation may cause the needle to impinge on the petrous ridge after penetrating the foramen. The needle is adjusted outside the foramen ovale until this orientation is obtained. The image intensifier is then rotated to the anteroposterior (AP) projection and aligned with the orbitomeatal line. This permits visualization of the internal auditory meatus through the orbit. The target site in this projection is a point approximately 9 mm medial to the lateral border of the internal auditory meatus. This point often coincides with the medial limit of the inferior dip commonly seen on the medial petrous ridge. When the needle is oriented in these two planes, methohexital is given, and the needle usually passes easily through the foramen ovale. A wrong skull-base foramen cannot be entered if they are used. It is at this point in the procedure that a marked rise in blood pressure may occur. Much more rarely, there is hypotension and bradycardia instead, which usually respond nicely to atropine. If the carotid artery is punctured while the surgeon is attempting to penetrate the foramen ovale, the needle is almost invariably too medial and too inferior in its location. This is usually an extracranial puncture, and it is not necessary to abandon the procedure if it occurs; it is merely necessary to reorient the needle and proceed. Usually, there are no complications from penetrating the carotid artery. Submentovertex Projection Some surgeons visualize the foramen ovale directly on the submentovertex projection and guide the needle accordingly. Hyperextension of the head on the neck to obtain this projection may not be well tolerated by the cervical spine of some elderly patients, and the radiographic technique is more cumbersome. Direct Visualization of the Foramen Ovale Others prefer to pass the needle through the foramen ovale using direct fluoroscopic visualization of the foramen. The head is hyperextended and rotated approximately 20 degrees away from the involved side. The image intensifier is angled approximately 40 degrees from the vertical and directed at the needle puncture site. The foramen is then directly visualized on the AP image intensifier. With flexion and extension of the head, the petrous ridge can be seen rising and falling behind the foramen. The needle is then passed through the foramen under direct vision. Revision to the AP projection would be recommended at this time. It has been recommended that an attempt be made to pass the needle through the medial aspect of the foramen. Localization of the Electrode in the Retrogasserian Rootlets When the needle has penetrated the foramen ovale. it is passed to the region of the clivus. at which point cerebrospinal fluid (CSF) is usually obtained. It is most desirable that there be a free flow of CSF from the needle. and the intent should be to place the electrode in the retrogasserian rootlets rather than the ganglion. If the cordotomy-type electrode is now inserted. the patient frequently flinches or grimaces as the electrode passes into the retrogasserian rootlets. This is a good sign that the electrode is in the proper place. The impedance is usually between 150 and 350 ohms when the electrode is properly positioned. although impedance measurement is not a necessary part of the technique. Impedances of 1000Ω or more indicate that the needle tip is in tissue. The most important and valuable indication that the electrode is in the proper position is a low voltage threshold to 50- to 60-Hz stimulation localized to the division to be treated. Electric-like paresthesias may be noted at 0.1 to 0.2 V; the lower the better. If more than 0.4 to 0.5 V is required, the electrode may have to be repositioned. It must be remembered that when very low voltage thresholds are obtained, the lesion may be made rapidly at lower current settings of the RF generator than would otherwise be required. If previous intracranial procedures have produced some sensory deficit in the face, somewhat higher voltages may be required before the patient notices the sensations. Rotation of the angled electrode within the LP needle may shift the response to the stimulation within the divisions or from one division to another. Changing the angle of the electrode may make the difference between no lesion and a very satisfactory one. This, along with adjustment in the depth of penetration, will aid in proper placement. It must also be remembered that at times the response to stimulation may be in one division although the lesion occurs in another. This is another reason to have the patient awake during the lesion making. The gasserian ganglion and retrogasserian rootlets lie on a plane running from superomedial to inferolateral, and keeping this in mind aids in electrode positioning. Sometimes a low-voltage response to stimulation can be obtained only by deflecting the electrode tip by holding the hub in a more superomedial or inferolateral position. The assembly can then be held in this position while the lesion is being made. Occasionally, the route through the foramen ovale is restricted by bony obstructions that limit manipulation of the electrode within the retrogasserian rootlets. If stimulation produces a motor response, the electrode is too medial. A further aid to electrode placement is the roentgenogram, which should always be obtained before making a lesion. AP projection through the orbits is of far more value than the lateral projection. Also, the AP image intensifier is constantly referred to during the procedure. AP projection will more consistently provide accurate localization. The reference point here is the relation of the electrode to the petrous ridge. If in the AP projection the electrode tip projects above (superior to) the petrous ridge, great care must be used lest the corneal reflex be lost, even if the response to stimulation is in the second division. Most lesions are made with the electrode at or a few millimeters below the petrous ridge in the region of the internal auditory meatus, as visualized through the petrous ridge. Lesion Making Cordotomy - Type Electrode The first lesion should be made with the RF generator at a low setting. Usually 10 to 12 V and 60 to 70 mA are used for the first 15- to 20-s lesion. If there is no resulting sensory deficit in the face, the lesion is enlarged with a 40-s lesion. If there is still inadequate numbness, the current is increased by 2 units and the 20- and 40-s lesions repeated until a vigorous pinprick is barely appreciated as painful. Another endpoint test that it has been found to be useful is to touch the face lightly with the twisted corner of a single layer of facial tissue. If the patient cannot feel the lightest touch of the point of this tissue but does feel the drag of the tissue across the face, the endpoint has been reached. Many operators prefer to use complete loss of pain (analgesia) as their endpoint. but this usually represents too much deficit. The final lesion is often made at approximately 18 V and 90 mA, though a higher current may be required. The surgeon should be prepared to make multiple incremental lesions until the desired sensory deficit is obtained. Intolerable pain is experienced when the electrode is in the ganglion or distal to it. and anesthesia is required to make a lesion there. A headache-type pain may be noted if the electrode burns the dura surrounding the retrogasserian rootlets. A burning type of tolerable discomfort in the face may be noted with the cordotomy-type electrode, especially when the final lesion is being made. This burning sensation is frequently noted lateral to the eye when a second-division lesion is being made and in or anterior to the ear with a third-division lesion. It is important to appreciate that with the smaller cordotomytype electrode and with the electrode proximal to the ganglion, the lesion is sometimes made with little or no pain in the face. This seems to be particularly true with first-division lesions. Neither the patient nor the surgeon may be aware that a permanent lesion has been made. If the corneal reflex is to be maintained, it is imperative, therefore, to insist that the patient tell the surgeon if discomfort is noted in the eye during lesioning, and also to constantly monitor the ciliary or eyelid reflex by repeatedly flicking the upper eyelid with a piece of twisted facial tissue while the generator is on. Often the first indication that this reflex is being impaired is a decrease in the consensual blink reflex and somewhat later there is a decrease in the direct blink reflex. Attention to this reflex is especially important when there is deep penetration of the electrode as noted on the AP projection. The first-division fibers are more sensitive to heat than those in the other divisions, and this fact is a warning. It has been possible to stop first-division pain and preserve the corneal reflex in almost 90 percent of patients with first-division pain by using these techniques in the awake patient. Preoperative counseling and planning are important here. Temperature-Monitoring Electrode When the electrode has been satisfactorily placed by the aid of stimulation and x-ray imaging, 35 to 45 mg of methohexital is given and, when the patient is asleep, the temperature is raised to 60°C for 60 to 90 s. The face is checked when the patient awakens, and if more numbness is required, additional lesions are made with increases of 5°C in temperature up to 80°C and sometimes 90°C. As with the smaller electrode, an attempt should be made to make multiple small lesions rather than one large one. This approach should not significantly prolong the procedure. After the initial lesion, which injures the nerve and reduces further pain, subsequent lesions should be made with the patient awake to permit sensory monitoring. General Principles 1. This is not a stereotaxic procedure but a free-hand skill that must be learned. The surgeon should not be in a hurry, and should schedule enough time to do the procedure properly. 2. The RF lesion is both current- and time-dependent and gradually increases in size over a period of about 40 s. After 40 to 60 s the lesion cannot be enlarged without increasing the current (milliamperage). 3. With either type of electrode, a flush may be noted in the area where sensory deficit is being created, but a dense lesion can be made with no flush. 4. Patients with multiple sclerosis and trigeminal neuralgia have twice the recurrence rate, and a more dense lesion is usually necessary. 5. Pain triggered from the second division but projecting into the first division requires treatment of the second division only. The first division need be treated only when there is a trigger site in the first division, which is usually from touching the eyebrow or hairline. 6. Before making the first lesion, the patient's face is checked with a pin, and the patient is told that the aim of the treatment is for the sharp, pricking quality of the pin sensation to be lost. The patient is also advised to inform the operator immediately if any pain or discomfort is felt in the eye while the generator is on. It is important to make sure that the patient is actually reporting loss of pain and not loss of touch; some patients lose track of what is wanted and lead the procedure toward loss of touch as an end point. An important question to ask is, "I know you can feel me touch you with this pin, but does it hurt?". 7. Each time the electrode is moved during the lesion making, the current settings on the generator must be returned to a low setting to avoid creating too dense a sensory deficit -one of the problems of the procedure. 8. By controlling the extent of sensory and motor deficits, it is possible to treat patients with bilateral pain without interfering with eating. 9. If difficulty is encountered in obtaining a low voltage threshold to stimulation or in making a lesion, it may be necessary to withdraw the needle to the foramen ovale and reinsert it in the direction where the lowest threshold to stimulation was obtained. Alternatively, it may be more expeditious to withdraw the needle from the skin and start all over again. Complications A consequence of too much numbness is a higher incidence of annoying paresthesia and dysesthesia in the face. Although 6 percent incidence of what the patient considered "annoying" paresthesia and dysesthesia after treatment. 53% of these patients still rated the overall results of the treatment as good to excellent. In 0.7% of patients, the dysesthesia was described as moderate to severe; in 3% it was considered to be severe, and in 0.4% to be intolerable. These sensations are often described as a burning, drawing, scratching, or itching sensation or, if the eye is affected, as feeling like sand or a hair in the eye. There is great variation in the individual response to numbness in the face. but most patients tolerate it well and are grateful provided the pain is relieved. It would appear that the incidence of annoying paresthesias and dysesthesias and of anesthesia dolorosa is higher in older and more emotionally unstable patients.
True anesthesia dolorosa occur in only 0.5 percent of patients. Now it is preferable to accept a higher recurrence rate, and to make multiple, less-dense lesions to reduce the incidence of annoying paresthesia and dysesthesia. Neurolytic keratitis may occur in some patients with corneal anesthesia, and meticulous eye care is required in the patient with an anesthetic cornea to prevent blindness. The corneal ulcers are more apt to occur soon after treatment than later. keratitis have place in (0.4 percent) and only two patients have lost vision. Fourth and sixth cranial nerve palsies have been reported following this treatment; they are usually transient. One transient fourth and one transient sixth nerve palsy. These palsies seem to occur more frequently with deeper and more medial penetrations, as for first-division lesions. A variable degree of trigeminal motor paralysis occur in 25% of cases. Most patients are unaware of the motor paralysis, even when it is complete, but some experience the sensation that the ear is "stopped up." This probably results from paralysis of the tensor veli palatini muscle. the function of which is to keep the Eustachian tube closed. Other patients may complain that their jaws do not meet properly or that their dentures do not fit. The patient should be reassured that these problems will pass, usually within 3 to 6 months. Two transient subjective and objective bruits on the side of the lesion were noted. These were probably small carotid-cavernous sinus fistulae. Large carotid-cavernous sinus fistulae have been reported. Post-treatment headache accompanied by moderate pleocytosis and negative cultures, which was presumed to represent a chemical meningitis. Meningitis is a recognized complication of this procedure and can rarely lead to death. Intracerebral abscess has been reported in 7 cases. Prophylactic antibiotics are recommended by some. The major problem with meningitis appears to be a failure to be aware of it as a possibility and to treat it immediately. Intracranial hemorrhage may occur in the form of subarachnoid hemorrhage or intracerebral hematoma from the hypertension previously described, or by direct puncture of intracranial vessels as a result of electrode malalignment. Herpes simplex eruptions occurred postoperatively in 31% of the patients, and these lesions can be severe. Nugent G.R. had two deaths in his series. One debilitated 89 year old man died 3 days postoperatively from pneumonia, and a second patient died of a myocardial infarction as she was leaving the hospital after an uncomplicated treatment. Upon discharge, the patient is counseled regarding tapering down the Tegretol or baclofen and is warned of the remote possibility of meningitis. If corneal sensation has been lost the patient and family are instructed to use artificial tears twice a day in the affected eye, to obtain a protective plastic shield to be attached to eyeglasses when in dusty atmospheres and, especially, to examine the eye daily for signs of inflammation. An ophthalmologist is to be consulted upon any suspicion of inflammation. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Notice: Not all operative activities
can be recorded due to lack of time.
WELCOME TO AL-SHMAISANI HOSPITAL
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
© [2016] [CNS CLINIC - NEUROSURGERY - JORDAN]. All rights reserved
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||






